Our research
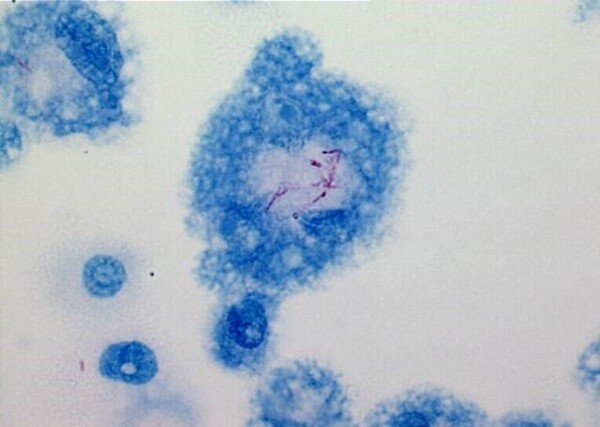
Our research group focuses on understanding specific immune responses in tuberculosis (TB), particularly how antimicrobial effector functions are induced and regulated in macrophages and T cells at the site of Mycobacterium tuberculosis (Mtb) infection. Research on clinical samples obtained from patient cohorts is integrated with well-defined cell and tissue models in vitro to explore pathogenic mechanisms in human TB.
Our research on the cellular and molecular interactions between bacteria and host cells have resulted in several discoveries of impaired immune responses in TB patients, which prevents effective killing of bacteria. Now, we exploit the acquired knowledge to restore Mtb-induced immune deviations and enhance imperative immune cell functions using a novel group of immunomodulatory compounds. A new component of this research is to sub-group TB patients based on immune endotypes, which will promote tailored treatment options and prevent the development of antibiotic resistance. For this work, the group has established clinical and research collaborations with TB-endemic countries such as Ethiopia and Bangladesh but also in Sweden, where some of the key concepts for host-directed therapies have been tested in randomized clinical trials.
The overall purpose of our research is to promote the development of next-generation individualized treatment options for different groups of difficult-to-treat TB patients.
Tuberculosis
Tuberculosis (TB) is caused by Mycobacterium tuberculosis (Mtb) and continues to be one of the world-leading killers among infectious diseases; every second a person in the world is infected with Mtb and every 25 second a person dies from TB.
Like several other bacterial infections, antimicrobial resistance (AMR) constitutes a serious threat to global TB control. Inadequate use of chemotherapy has resulted in resistance of Mtb to most known antibiotics and increased rates of multidrug-resistant TB (MDR-TB) with low treatment success rates. Host-directed therapies target multiple immune pathways to enhance cure, while reducing disease severity, side effects and problems with drug-resistance. The importance of the immune response in TB control is highlighted by the increased risk of TB in primary immunodeficiencies, HIV infection and upon treatment with TNF-α inhibitors.
Key collaborations
Karolinska Institutet and Karolinska University Hospital
- Ass. prof. Magda Lourda, Dept of Laboratory Medicine
- Assoc. prof. Lina Davies Forsman, MD PhD, Dept of Medicine, Solna
- MD PhD Hilmir Asgeirsson, Dept of Medicine, Huddinge
- Prof. Peter Bergman, Dept of Laboratory Medicine
Sweden
- Linköping University, Department of Clinical and Experimental Medicine
Prof. Maria Lerm, PhD Sadaf Kalsum, and Prof. Thomas Schön
International

- Addis Ababa University (AAU) and Black Lion University Hospital, Ethiopia:
Dr. Amsalu Bekele, Dr. Wondwossen Amogne, Dr. Endale Kassa and Prof. Getachew Aseffa - Armauer Hansen Research Institute (AHRI), Ethiopia:
Assoc. prof. Abdissa Alemseged (Scientific Director of AHRI) - International Centre for Diarrhoeal Disease Research (icddrb), Bangladesh:
PhD Rubhana Raqib

