Research focus
Survival and infectiousness of Mycobacterium tuberculosis after aerosolization
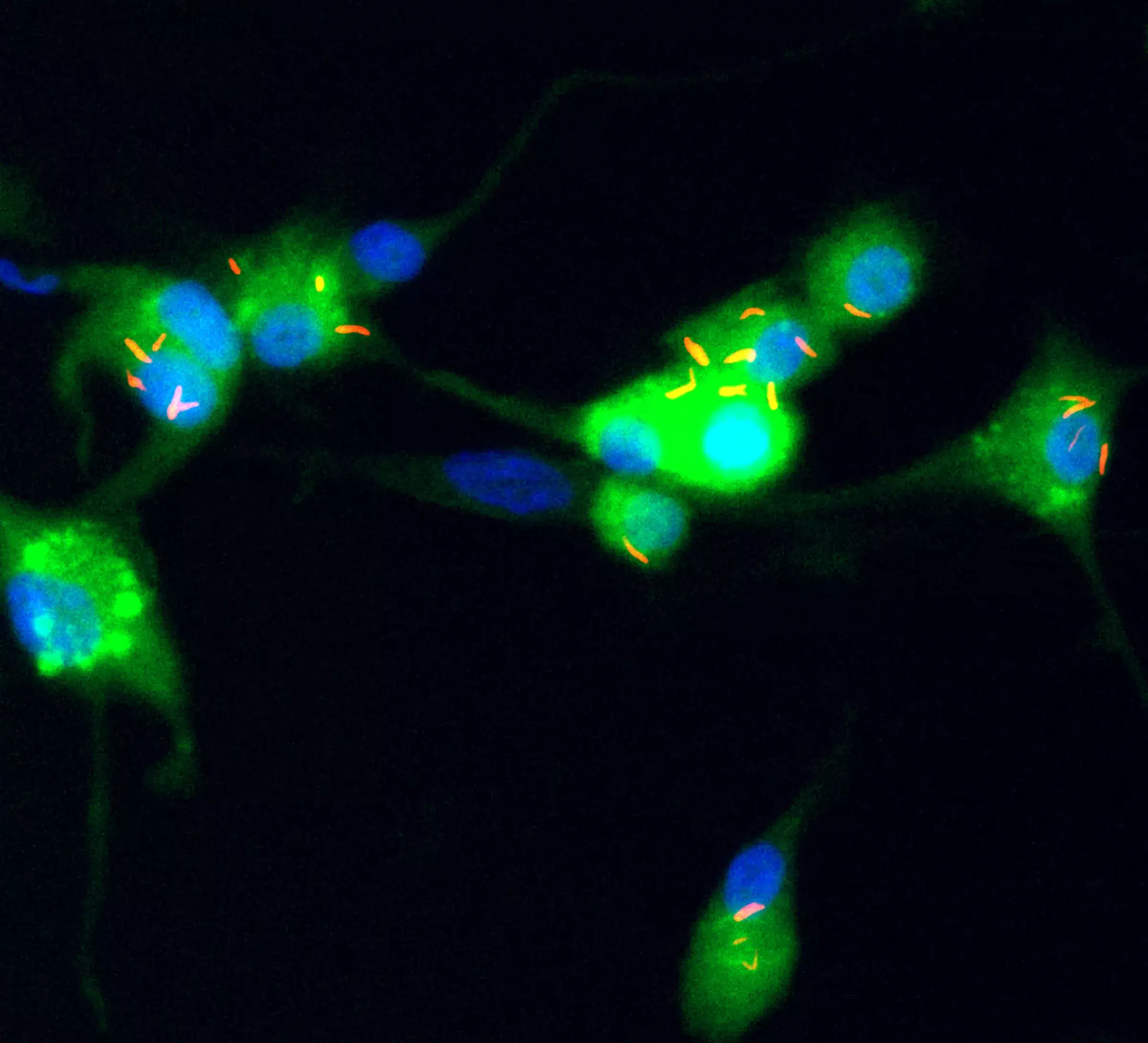
Tuberculosis (TB) is transmitted when aerosols carrying Mycobacterium tuberculosis are inhaled into the lung and infect macrophages lining the alveoli. A caveat for the success of this cascade is that the bacilli can cope with aerosol stress and survive long enough in open air before they can be inhaled. Extended time in aerosol also stands to impact the infection potental of the bacilli in macrophages. The ability of M. tuberculosis to remain viable and infectious in aerosol is therefore a key determinant for its transmission.
We are investigating if there are specific environmental conditions that support or mitigate the cultureability and infectiousness of M. tuberculosis in aerosols. We are also investigating if extended aerosol dwelling reduces survival and infectivity of M. tuberculosis; if aerosol transpor triggers specific gene-expression in M. tuberculosis, and finally, if the success of highly-transmissible community isolates of M. tuberculosis is linked to their ability to endure aerosol transport.
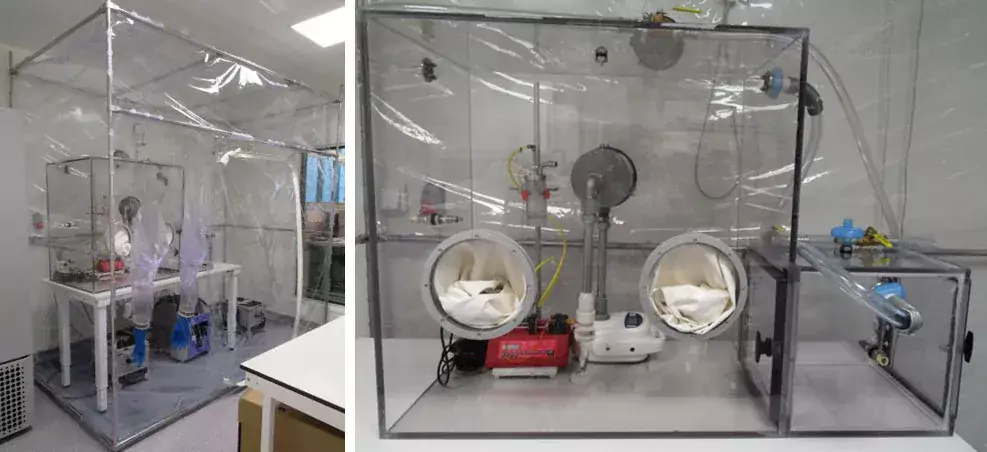
We have set up a unique aerobiology platform in BSL3 to address these important knowledge gaps in tuberculosis transmission. This platform and its trained personnel also support Swedish pandemic laboratory preparedness with capabilities to study the aerobiology of new and emerging pathogens.
Results from this research will contribute important new information on conditions that mitigate transmission of airborne M. tuberculosis, and provide novel insights on mycobacteria-macrophages interactions.

Detection of M. tuberculosis in cough aerosols
Aerosols carrying M. tuberculosis are released during coughing by persons with active pulmonary TB. These infectious aerosols can remain airborne for extensive periods of time. Detection of M. tuberculosis in aerosols can help break the chain of transmission by identifying infectious persons and community hotspots of transmission. Tools that are easy-to-use and scalable in low-income, high-burden countries are however lacking.
With this in mind we have developed a small, low-cost electrostatic air sampler that can be used together with nucleic acid amplification tests to detect M. tuberculosis in aerosols. We are investigating the performance of this device at collecting aerosolized M. tuberculosis from TB patients in Sweden and South Africa. By comparing M. tuberculosis detection in cough with routine sputum diagnostics we can discern the feasibility of using cough as a diagnostic for TB. In a clinical aerobiology platform at Stellenbosch University, South Africa, we are stratifying detection on our low-cost sampler with validated readouts for TB infectioussness in patients.
Our air sampler has recently been used to demonstrate infectious SARS-CoV-2 in the air from hospital rooms housing COVID-19 patients. It is currently being tested as a monitoring device for respiratory viruses in sheltered housing for the elderly.
Results from this research will inform on the use of cough as a novel TB diagnostic specimen, and detection of M. tuberculosis in cough as an estimation of transmission risk.
Support our research
 Photo: Chokniti Khongchum
Photo: Chokniti KhongchumMake a donation to our research at MTC
Your support means a lot to our success. This allows us to go further in our efforts to improve human health through research and education.
Read here how you can make a donation via Swish.