Our research
Using state-of-art methods we are looking into γδ T cell reconstitution, and how these cells are affected by different transplant related factors. We also aim to investigate the development and functionality of γδ T cells in detail after hematopoietic stem cell transplantation (HSCT). This could help pave the way for more advanced and targeted approaches in cancer immunotherapy and in infectious diseases, particularly in patients undergoing HSCT.
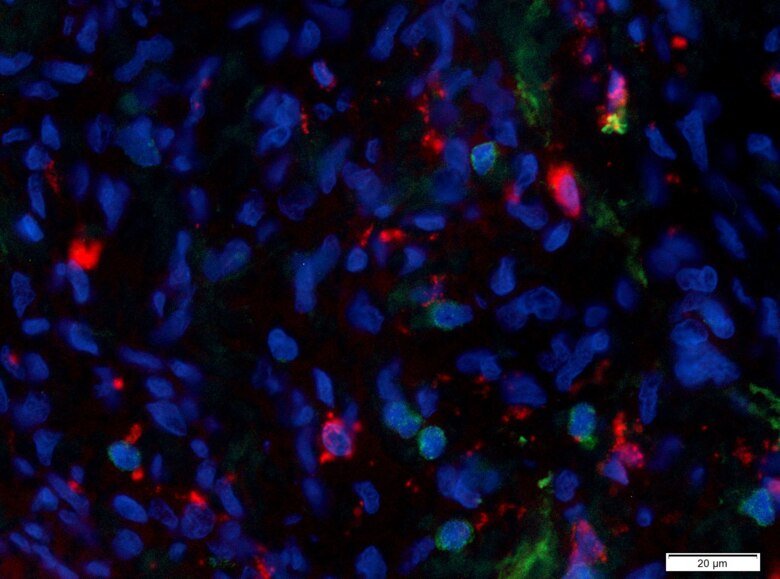
We also have projects focusing on tumor-infiltrating lymphocytes (TILs) in solid tumors, mainly in ovarian cancer and prostate cancer. We use cancer patient-derived material and isolate lymphocytes from peripheral blood, ascites and tumor which we use for projects involving the characterization and functionality of lymphocytes with emphasis on T-cells. Our aim is to increase the understanding of how the tumor microenvironment can alter the phenotype of TILs and their ability to function and eliminate tumor cells. By using different immunomodulatory approaches, including PD-1 blockade with novel constructs, we try to enhance the responsiveness of TILs ex vivo.
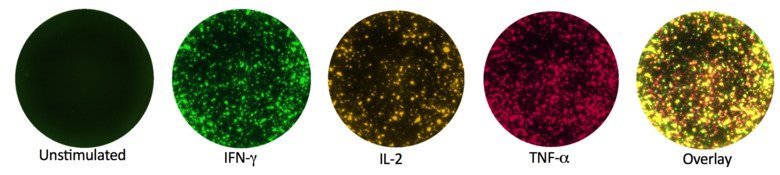
Acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) are diseases which require treatment with toxic chemotherapy or HSCT. A high burden of leukemic stem cells (LSCs) in AML/MDS patients is associated with high risk of relapse and death, making those cells a good target for new therapies. Bispecific T-cell (BITE) and NK-cell engagers (BIKE) are new classes of immunotherapeutic agents. Their structure and specificity allow them to link a T-/NK-cell to a tumor cell and thereby stimulating effector cell activation, tumor killing and cytokine production. One project within the group is focused on the design and characterization of a BITE and BIKE directed against the molecules expressed LSCs. Our BITE/BIKE would enable the redirection of the T-cell effector function towards malignant cells, directly targeting leukemic cancer cells. The specific depletion of LSCs in AML/MDS patients making the therapy more efficient and less toxic.