On the way to healthier lungs
Lung cancer is the fifth most common kind of cancer in Sweden and strikes far fewer than half as many people every year as prostate cancer or breast cancer, which top the list. In spite of this, lung cancer is the type of cancer that by far kills the largest number of Swedes every year.
Text: Fredrik Hedlund, first published in Swedish in the magazine Medicinsk Vetenskap No 1/2018
THIS IS BECAUSE the prognosis is so bad. More than 4,000 people were diagnosed with lung cancer in 2015, while the mortality rate for lung cancer that same year was just over 3,600 people (compared with around 2,350 people dying from prostate cancer and more than 1,400 from breast cancer). On average, just over half of those diagnosed with lung cancer are alive one year later and the five-year survival rate is as low as 15 per cent.
The main reason for the bad prognosis for the disease is that it is often discovered too late when the tumour in the lung has already developed and begun to metastasise, sending secondary growths around the body. The average age at diagnosis is around 70, but lung cancer also strikes younger people. In 2015, around 90 people younger than 50 were diagnosed with lung cancer.
After long having been a disease that overwhelmingly struck men, the gender distribution has changed in recent years. In 2012 and 2013, the age-standardised risk was the same for men and women and lung cancer has since become more common among women than men. As early as 2005, lung cancer surpassed breast cancer as the type of cancer that kills most women in Sweden.
Smoking habits 30-40 years ago
Lung cancer is closely linked to smoking and 85-90 per cent of everyone diagnosed are smokers or former smokers. This is something that has also created a stigma around the disease where those afflicted often blame themselves for being struck at the same time that it was previously difficult to free up research funding for lung cancer research. This is something that is now changing.
The gender differences in the diagnosis trend are also very much reflected by smoking habits in the population 30-40 years ago. Among men, smoking was most common in the 1960s when around half of all men smoked. The peak among women instead occurred in the 1980s when about one in three women smoked. The percentage of smokers decreased earlier among men, which is now being seen in the lung cancer statistics. But the total number of men in Sweden diagnosed has not gone down even though generally fewer men smoke.

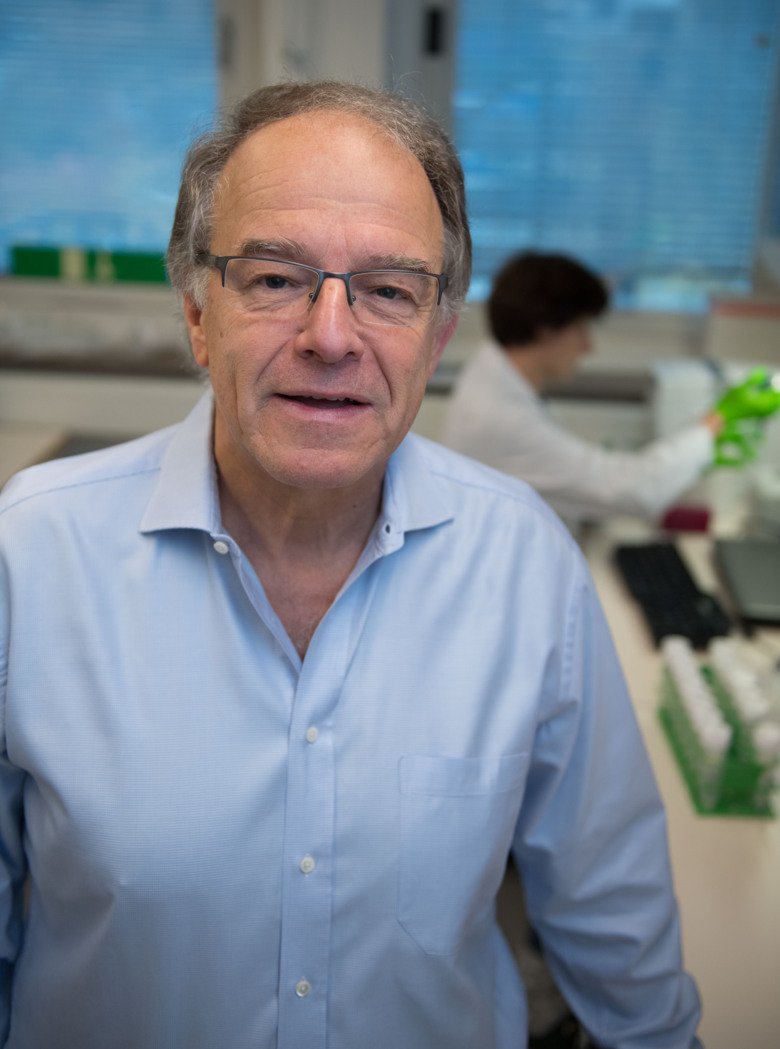
“This is related to us living increasingly longer and more people having time to get the disease, which means that we have had a somewhat stable situation since the 1970s,” says Per Gustavsson, Professor of Occupational and Environmental Medicine at the Institute of Environmental Medicine, Karolinska Institutet.
His research focuses on the risk factors for lung cancer other than smoking, mainly in the work environment, but also in air pollution in a public environment. He emphasises that lung cancer in some cases can be traced to combinations of several different causes.
We find the second largest risk factor for being struck by lung cancer at home.
“Radon in homes contributes to around 500 cases of lung cancer every year,” he says.
Exposed to radon
But here too, the lead times are long so that those diagnosed now were exposed to radon 20 to 40 years ago.
“The limits for radon levels in residential buildings have since been lowered so with the radon levels we have today, the risks are lower,” says Per Gustavsson.
In terms of risks in the work environment, they have mainly been studied among men since it has most often been men who have had jobs that entail exposure to risk factors for lung cancer, such as construction, masonry and mining.
“Between 15 and 25 per cent of the lung cancer cases among men can be attributed to the work environment since they could be avoided if the exposure were removed from the work environment. So that’s a lot,” says Per Gustavsson.
Facts: Glandular cancer common
Lung cancer is broken down into several sub-groups depending on appearance and placement in the lungs.
- Non-small cell lung cancer. 85 per cent of all lung cancer cases.
- Adenocarcinoma. Most common form of lung cancer. Also called glandular cancer since it grows from glandular cells in the lungs.
- Squamous cell carcinoma. Second most common form of lung cancer. Begins in the bronchi.
- Small-cell lung cancer. 15 per cent of all lung cancer cases. Grows quickly and has often spread at discovery. Almost only strikes smokers.
Lung cancer is divided into four stages, which among other things takes into account tumour size, if the lymphatic system is affected and if the cancer has spread.
- Stage I. A limited tumour that has not spread outside the lung or bronchi.
- Stage II and III. Cancer cells are in one or more lymph nodes.
- Stage IV. Cancer is spread with metastases in other organs.
The probably most well-known work environment risk that causes lung cancer is asbestos, the fibres of which get stuck in the lungs and cause the development of tumours, among several other health hazards. The material was already discovered to be unhealthy early in the 20th century, but the use of asbestos was not banned in Sweden until 1982. But this does not mean that the problem is gone. It is still in the buildings where it was used before the ban. Buildings that are now beginning to be renovated. Then it is important that those responsible for the renovation know if asbestos is present, which does not always seem to be the case, according to Per Gustavsson.
“For example, when plumbing upgrades are to be made to buildings from the 1950s and 1960s, asbestos can be present in the tile fasteners in the bathrooms. When the old tile is broken off, the construction workers can be exposed to asbestos. For every new building, samples must be taken and sent for analysis to see if asbestos is present or not – if asbestos is there, special safety rules apply – and this might not always be followed. Patients and people in the construction industry provide this picture in any case,” says Per Gustavsson.
The fact that asbestos, 35 years after the ban, is still the foremost work environment-related cause of lung cancer shows how slowly preventive measures have an effect on the development of lung cancer. But there are also risk factors that have not been eliminated from workplaces and public environments. The most important of them is stone dust or quartz that in working life can be found in the construction industry, in masonry and in tunnel construction, for example.
“In professional life, it is an exposure that really needs to be reduced. The Swedish Work Environment Authority has proposed a reduction of today’s limit by half, but interests among labour market parties question this,” says Per Gustavsson.
Caused by diesel exhaust
Another risk factor that exists both in professional life and in the urban environment is diesel exhaust. It was categorised as carcinogenic as recently as 2012. But in spite of this, it is a little unclear how hazardous it actually is today. The cases of lung cancer caused by diesel exhaust that the doctors see now are due to exposure long ago and both the diesel fuel and engines have improved since then.
“It takes 20-30 years to get lung cancer both from smoking tobacco and from diesel. However, when we see that this is a strong carcinogenic factor now, we don’t know how large the risk is in environments exposed to diesel today; it depends on how well diesel technology has been able to be developed,” says Per Gustavsson.
Something that is naturally of significance to how much concern there should be for diesel exhaust in the city.
“In the city, it is a combination of street dust, which partly contains quartz, and traffic exhaust, where we have both diesel and petrol. We previously also had home heating where people made fires in stoves in the city, as was done in the 20th century and created high levels of air pollution,” says Per Gustavsson.
According to the latest Environmental Health Report from the Swedish Public Health Agency and Karolinska Institutet from 2017, average life expectancy in Sweden is estimated to be shortened by an average of six months due to air pollution, more in the south than in the north and more in urban areas than in the countryside. In terms of lung cancer in particular, there is a study from 2000 that indicates that up to one out of ten cases of lung cancer in Stockholm could be due to air pollution from the traffic 20 years earlier, but this estimate is said to be uncertain.
Non-small cell lung cancer dominant
Lung cancer is broken down into small-cell and non-small cell lung cancer where the latter is completely dominant and accounts for 85 per cent of the cases. Non-small cell lung cancer is in turn divided into three sub-groups: adenocarcinoma (or glandular cancer), squamous cell carcinoma and large-cell carcinoma. Doctors also divide tumours into different stages depending on size and spread (see fact box).
A major reason for the bad prognosis with lung cancer is that the tumours are discovered too late, when they have already developed to the later stages and when it is no longer possible to surgically remove them. But for tumours discovered in early stages, the prognosis is good and an operation before the tumour has spread is today one of few ways to cure the disease. But this is changing. In the past decade, knowledge and possibilities of treating lung cancer have been dramatically improved.

“From having treated all lung cancer in roughly the same way, with chemotherapy, we have now discovered that the disease can be broken down into sub-groups depending on what mutations there are in the tumour. And new pharmaceuticals have also been developed that can go in and block these signals in the tumours, often with very good effect,” says Simon Ekman, Senior Physician at Karolinska University Hospital and Docent at the Department of Oncology-Pathology, Karolinska Institutet.
The doctors take samples of the tumour and apply treatment to the patients who have variants of lung cancer with mutations that are treatable. The new treatments are also significantly easier for the patients to take compared with chemotherapy since they are taken in tablet form at home and they mostly also do not have as many side-effects since they are targeted on the tumour cells.
“This is a clear gain for quality of life. Compared with chemotherapy, it provides better quality of life, tumour response and life expectancy,” says Simon Ekman.
Resistance to the treatment
The mutations that the treatments are targeted on are only behind around one fifth of the lung cancer cases in Sweden. About 12-15 per cent of the patients have a mutation in a growth receptor called EGFR (Epidermal Growth Factor Receptor), 4-5 per cent have a mutation called ALK (Anaplastic Lymphoma Kinase) and 2 per cent have a mutation called ROS1, but a great deal of research is under way to find treatments for more mutations,” explains Simon Ekman.
“So we can expect new treatments against new sub-groups to be identified soon. At present, it is estimated that around 70 per cent of all lung cancer cases have such a driving mutation,” he says.
However, one concern is that the good effect of the targeted treatments does not seem to last. The tumour eventually develops a kind of resistance to the treatment.
“Sooner or later, virtually all patients can be said to have an increase in the tumour again. It may be after a number of years, but it can also happen faster. And it is then a kind of resistance mechanism where a part of the tumour developed in a different way and avoids the blockade that has been applied,” says Simon Ekman.
But then a new sample can be taken and in some cases a new targeted treatment can be applied. Development is going quickly and the targeted treatments now exist in several generations with slightly different active mechanisms that have proven successful when the tumour becomes resistant to earlier treatments. Development is right now a kind of race between the researchers and the tumours. Simon Ekman’s own research is, among other things, about trying to find the genetic changes that lead to resistance and find out why it develops in the patients. The goal is to be able to find new ways to attack resistance development.
Hijack the immune system
But there is more good news in terms of the treatment of lung cancer. Even newer than the targeted treatments is something called immunotherapy. Researchers have found that tumours often have a way of avoiding attacks from the human immune system that can be disrupted. The tumour cells can hijack the immune system by binding to a receptor on some of the immune system’s cells and thereby neutralise the immune system’s possibility of attacking them. The new pharmaceuticals target either the receptor on the immune system cells with the slightly dramatic name programmed cell death protein PD-1, or the programmed death ligand PD-L1 that is on the surface of the cancer tumour. The aim is to block the binding and not allow the tumour to evade the immune system.
The medications were first approved for skin cancer in 2014 and have reduced mortality from skin cancer dramatically. Then they were tested and approved for the treatment of lung cancer.
“You could say that this is also a kind of targeted therapy in that it targets a specific immune factor, but it is significantly broader since it mobilises somewhat large parts of the immune system. Even if the medication is targeted on a specific factor, it triggers an immunological chain reaction that works on a broader group of patients,” says Simon Ekman.

For some patients, the effect is very good. Depending on which immunotherapy is given, between 20 and 45 per cent of the patients have a direct tumour response where the tumour shrinks, others have a stabilisation of the tumour’s development while some do not have any greater effect at all. Why some tumours respond and others do not is not really known, but intensive research is being conducted on this. A great deal of research is also being conducted on the possibility of combining different treatments.
“An important part of the development is finding combinations that provide even better responses than just a single treatment. A number of different studies are under way with combinations of targeted treatments and immunotherapy and chemotherapy. In the field of lung cancer along, there are up to 360 different immunotherapy studies under way and in terms of all kinds of tumours, more than 1,800 studies are under way, so it is an enormous effort,” says Simon Ekman.
An extra push to the world’s cancer research will undoubtedly be given by what can be seen as cancer research’s own Nobel Prize. The successful Swedish businessman Bengt Sjöberg died from lung cancer in January 2017, at the age of 68, without ever having smoked a single cigarette. Before he died, he had formed a foundation to which he donated most of his fortune – SEK 2 billion – for use within cancer research. It is the largest single donation to research ever made in Sweden, even larger than Alfred Nobel’s donated fortune that would be SEK 1.7 billion translated into today’s monetary value. Like the Nobel Prize, the Sjöberg Prize will be awarded annually and the prize amount is the same, USD 1 million. The very first Sjöberg Prize was awarded in 2017 to the two American researchers Tony Hunter and James Allison whose research is behind the development of the targeted medications and immunotherapy.
More efficient radiation methods
In the midst of all of these new, praised treatments, an older form of treatment also has an important role in the treatment arsenal. It is radiation therapy that has been significantly improved in terms of precision, which both means more efficient radiation methods and fewer side-effects. In addition, in parallel with this development, the image reproduction technology has also been refined, which contributes further to the higher precision of the radiation therapy. This precision radiotherapy, which is also called stereotactic radiotherapy, is developed at Karolinska University Hospital.
“Clinics and physicians at Karolinska University Hospital were the first in the world to show that it was possible to provide stereotactic radiotherapy that kills the tumours,” says Rolf Lewensohn, Professor of Oncology at the Department of Oncology-Pathology, Karolinska Institutet and Senior Physician at the Department of Oncology at Karolinska University Hospital.
It involved lung cancer patients whose cancer is discovered early in stage 1, but who, for various reasons, cannot undergo surgery.
Precision radiotherapy is a technology that has now grown globally and is used throughout the Western world at the hospitals that have the advanced radiotherapy facilities required.
Rolf Lewensohn and his group have gone further with the radiation technology and are now developing methods to irradiate metastases to also be able to treat patients at a later stage with precision radiotherapy.
“We have developed possibilities to irradiate metastases that are in the liver, in the adrenal glands, in lungs and even in the vertebra. For limited metastasis, we believe that we can extend the time to a relapse through such radiation, extending the life of the patient,” he says.
Studies are now also under way where precision radiotherapy is combined with immunotherapy where the idea is that the radiotherapy triggers the immune system,” explains Rolf Lewensohn.
“We don’t dare speak of a cure yet because we first have to understand which patients it could apply to. But what we are hoping for is to be able to achieve a several years longer life, with mild side-effects so that it really provides quality of life,” he says.
Various methods to screen those at risk
But despite all of the good treatment news, a major problem is still that lung cancer in the majority of the cases is discovered late when the tumour has already advanced to the lymph nodes and sometimes also formed metastases and is harder to treat. One has therefore long talked about various methods to screen those at risk to be able to discover the tumours earlier. In the 1980s, screening studies were done with lung X-ray that could not show any increased survival. In 1999, the first study came where low-dose computerised tomography was used instead, which could show better effectiveness in finding the patients, but it has since been debated if screening activities could really reduce mortality.
Ever since 2011, when the study “National Lung Screening Trial”, NLST, was published. There, more than 53,000 heavy smokers in the U.S. were screened over three years’ time and the study was able to show a 20 per cent lower mortality from lung cancer. The decrease in the total mortality was indeed only 6.7 per cent, but it was enough for U.S. authorities in 2013 to recommend annual screening of heavy smokers and former heavy smokers between the ages of 55 and 74.

In Europe, the national authorities are still waiting on a study from Belgium and the Netherlands called Nelson, where just under 16,000 heavy smokers and former heavy smokers were allotted to screening with low-dose computerised tomography or not. The results are expected to be presented this year or next year and are what will probably determine if screening will be introduced in Europe as well.
“If it is positive, there is really no doubt, but if it shows anything else, one will have to think about it. I absolutely believe that we will ultimately end up there with some kind of screening,” says Simon Ekman.
Damage through overdiagnosis
And his view is backed up by a European expert group on screening for lung cancer that in December 2017 published a so-called “EU position statement” where they recommend the EU member states to begin planning for an introduction of lung cancer screening within four years.
The question may seem simple. Screen heavy smokers and reduce lung cancer mortality by 20 per cent. But there are quite a few factors to consider. The screening programme can in itself cause some damage through overdiagnosis, unnecessary examinations and operations on benign tumours, psychological suffering and the extra radiation that the participants are exposed to. Psychological suffering in particular can become tangible since a whole 96 per cent of those who were first suspected of having lung cancer proved to be false positives, meaning they did not have lung cancer, in the U.S. study.
“We will discover a lot of spots on lungs that need to be monitored for several years, most of which will never develop into cancer. It may become a resource issue how these should be monitored and by who,” says Simon Ekman.
In the resource struggle, it is important that the view of lung cancer as something self-inflicted does not negatively affect the decisions, according to Simon Ekman.
“We are working hard to remove the stamp of shame around the disease and I believe it is beginning to subside. Of course, it is a cost to society on the other end if people get sick; it costs a lot to take care of an advanced lung cancer. In that sense, it is a benefit to try to keep people healthy,” he says.
Identify and evaluate biomarkers
But there are also other ways to both find and monitor tumours. If extensive research is under way to identify and evaluate so-called biomarkers, proteins or genes that can reveal that a tumour is there and also be able to show at all the tumour’s origin and sensitivity to treatment.
The most spectacular future visions speak of being able to find tumours very early and with great precision by analysing exhaled air or various bodily fluids.
But right now, the objective is to find biomarkers in the blood, which can identify mutations that can guide the treatment and also determine if the treatment is effective or not.

“Several different kinds of biomarkers can be found in the blood. It may be circulating tumour cells, DNA from the tumour or isolated proteins that are expressed in the tumour that have been cut off or freed through cellular degeneration,” says Katalin Dobra, Senior Physician at Karolinska University Hospital and Docent in Molecular Pathology at the Department of Laboratory Medicine, Karolinska Institutet.
She looks for new biomarkers both for early diagnostics and to predict response to various treatments.
“How early a tumour can be discovered most often depends on the tumour burden and how many tumour cells are found in circulation. Therefore, it is often only when it is a somewhat advanced tumour that it can be found,” she says.
Due to this, among other things, researchers are working to identify more and more sensitive biomarkers.
“In the future, we hope to be able to map the entire protein profile, the DNA profile or the mutation profile and from that, draw conclusions on diagnostics and treatment. There are growing numbers of markers that we are trying to combine. Now, we have identified up to 20 different markers that we will combine,” says Katalin Dobra.
In the future, she believes in combinations of even more biomarkers of various kinds. Not least to be able to increase sensitivity and identify when the tumour has developed resistance to targeted treatments and to know what treatment should then be applied instead.
Signal system for growth factors
At the same time a great deal of research is being done at universities and in the pharmaceuticals industry to find new approaches to lung cancer tumours. One of those who are looking is Kristina Viktorsson, researcher at the Department of Oncology-Pathology at Karolinska Institutet. She has studied a special signal system for growth factors in lung cancer and together with her research team she discovered that a collection of receptors (Eph-receptors) and ligands (Ephrins) are active in lung cancer.

“If the expression of the Ephrin ligands are modulated, the lung cancer cells’ ability to survive can be changed, which indicates that this network has a driving function in lung cancer,” she says.
In addition, the signal system seems to play a role in resistance development against EGFR treatment.
“Patients who become resistant to EGFR treatment have among other things proven to have higher signalling through Eph-receptors, which indicates that there should be something there clinically as well,” she says.
The system also appears to be able to influence the tumours’ ability to send out secondary tumours, metastases, something that could be of major significance in the future.
“At present, we are focusing on how we can affect the system to counteract resistance development in EGFR treatment, but it is clear that the ultimate objective is to be able to slow metastasising,” she says.
Kristina Viktorsson has conducted research in the lung cancer field for around 15 years and seen the entire development that has taken place with targeted treatments and immunotherapy. As a molecular cancer researcher, it is an interesting and stimulating time to work in, according to her.
“Incredible advances have really been made in the past ten years. For some patients, lung cancer has become a chronic disease instead of a death sentence, but we need to know a lot more about the individual patient’s tumour to be able to individualise the treatment,” she says.
