Research at the Center for Infectious Medicine (CIM)
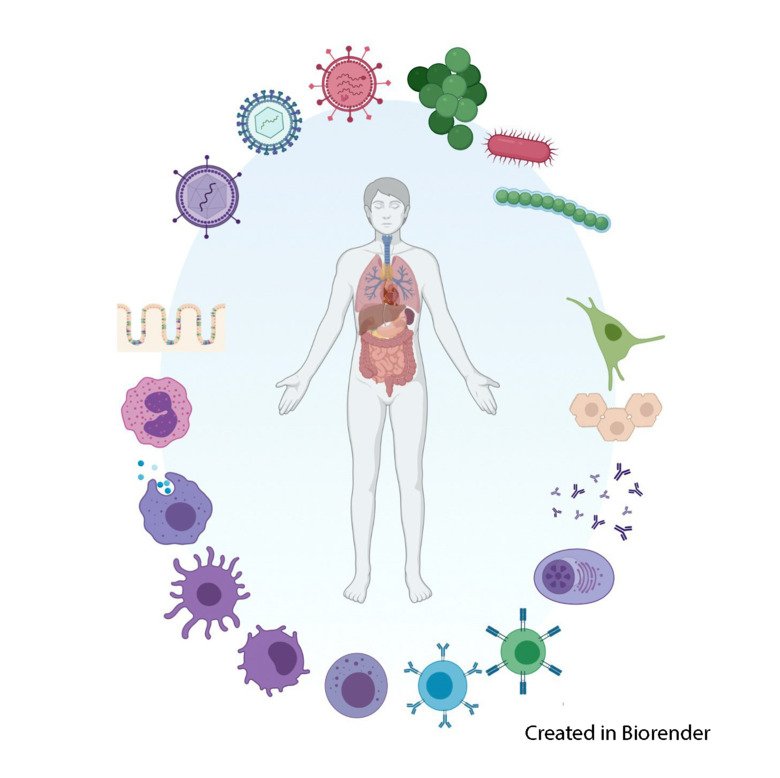
To tackle many of the problems that several infectious diseases impose, we need a better understanding of the human immune system and immune reactions towards pathogens in humans. Studying functional diversity of the human immune system, in particular innate immune cells and lymphocytes, is highly prioritized at the Center for Infectious Medicine (CIM).
Research objectives
The research at the Center for Infectious Medicine (CIM) can be divided into four main objectives:
1. To advance our understanding of the human immune system at a cellular and molecular level
Decades of intense cellular and molecular studies have resulted in the identification of components of the immune system. Studies of the mouse immune system, most particularly through the use of animals with targeted gene inactivation, have permitted linking these components to specific functions in immunity. In spite of this progress, the study of the human immune system has lagged behind that of the mouse. Improvements in technologies and reagents, however, now permit detailed analysis of the human immune system at cellular and molecular levels. Such analyses are crucial for furthering our understanding on how the human immune system combats infectious diseases and cancer.
2. To advance our understanding of immune reactions to pathogens in humans, and pathogen escape from immunity
With a clearer insight into functions of the human immune system gained through basic research as well as the development of new techniques, we can now address fundamental questions relating to host immune reactions to human pathogens and strategies employed by pathogens to evade immunity, at a level not previously conceivable. Improved understanding of host immunity to human infection set the stage for development of new intervention strategies such as, e.g., new vaccines.
3. To develop new immunomodulatory prevention and treatment strategies for human infectious diseases
Although many approaches to producing new vaccines have been initiated, systematic evaluation and optimization have proceeded slowly, in part because of factors such as the expense and complexities in advancing new candidate vaccines into phase I/II trials and scientific challenges.
Importantly, techniques for eliciting immunogenicity in new vaccines are lacking and sorely in need of complementary, safe adjuvants to help them reach full potential. Likewise, antigens must be optimized to yield the strongest possible immune responses. Vaccine-oriented projects focus particularly on optimizing strategies for TBE, yellow fever and enterovirus vaccination. However, several efforts presented here are equally applicable to vaccines against other major pathogens, e.g., HCV, influenza virus, and M. tuberculosis.
4. To test new immuno-modulatory prevention and treatment strategies in clinical phase I/II trials
The 21st century has witnessed a need to move research results more quickly to clinical settings. Clinical research helps to assure that new diagnostics, treatments and intervention strategies are safe and effective. Currently, this is a lengthy and sometimes (if not often) inefficient process. Meeting these demands requires new and more efficient processes from discovery to clinical validation of research results in humans. Researchers at the center are conducting pre-clinical and clinical trials involving the testing of novel vaccine combinations and enterovirus vaccines. Studies are also going on aiming at developing adoptive immunotherapy protocols with NK cells against specific malignancies.
Research competence areas
The research groups at CIM are divided into several specific research competence areas. However many of the groups are active within several areas, and all research groups at CIM are active in the Tissue Immunology research area.
Tissue Immunology
The Karolinska K/KI COVID-19 sample collection
The Karolinska K/KI COVID-19 sample collection for researchers contains clinical samples from >300 patients, with 1-4 samples per patient. Preserved whole blood, plasma, serum, PBMC and DNA, is available for research.

- Substantial clinical and experimental metadata is linked to the sample collection and available for research upon request and approval.
- The clinical samples are stored within Stockholms Medicinska Biobank (Stockholm Medical Biobank).
NOTE! Presently detailed information about the Stockholm Medical Biobank is available in Swedish only.
The Karolinska K/KI COVID-19 sample collection was established during 2020-2021 as a collaboration between the Center for Infectious Medicine (CIM), the Department of Infectious Diseases and the Department of Intensive Care of the Karolinska University Hospital.
