New help for widespread disease
Diabetes is not simply one disease, but several; each with different causes, prognoses and treatments. When it comes to the disease, there are still many missing parts to the puzzle. Despite this, treatment has evolved tremendously over recent decades. And now, the diabetes map may be on the verge of being completely redrawn.
ON 1 MARCH THIS YEAR, researchers at the Swedish universities of Lund, Gothenburg and Uppsala, as well as a number of Finnish universities, published an article in the scientific journal The Lancet Diabetes & Endocrinology in which they proposed an entirely new division of diabetes diseases. Because diabetes is not simply one disease, but several, each with different causes, prognoses and treatments; something that doctors and researchers have long been aware of. The question is: how should the various diseases be defined?
Diabetes was initially viewed as a single disease characterised by abnormally high blood sugar levels. The first active treatment for this condition was introduced in 1922, in the form of insulin.
However, in 1936 an article was published in the medical journal The Lancet demonstrating that one group of diabetes patients were sensitive to insulin, while another was not. The conclusion of the article was that, while one type of diabetes was caused by a lack of insulin, the other was the result of a lack of some other unidentified factor that makes the body sensitive to insulin.
And they were not entirely wrong. Today, researchers consider type 1 diabetes to be an autoimmune disease in which the patient’s own immune system, for some unknown reason, attacks and kills insulin-producing beta cells in the pancreas. So, type 1 diabetes is indeed caused by insulin deficiency. The disease normally presents during childhood between the ages of 5 and 14.
However, another type of autoimmune diabetes has also been identified, caused by an immunological reaction, in which the disease instead presents in adulthood; a slower version of type 1 diabetes known as latent autoimmune diabetes in adults (LADA).
The other kind of diabetes described in the Lancet article of 1936 – the one that failed to respond to insulin treatment – is included in what we now call type 2 diabetes. However, the underlying causes remain unknown, although it is unlikely that a lack of some unknown factor makes the body sensitive to insulin. Instead, doctors and researchers are in some agreement that what we refer to as type 2 diabetes does not have a single cause and is not simply a single disease.

“We must stop looking at type 2 diabetes as a single disease and instead see it as a syndrome including many forms of diabetes,” says Mikael Rydén, professor of clinical and experimental fat tissue research at Karolinska Institutet’s Department of Medicine, Huddinge and senior physician at Karolinska University Hospital.
This is also a fundamental concept behind the new proposal to divide type 2 diabetes into four groups depending on severity and other characteristics.
“The article confirms that, at a genetic level, there are various forms of diabetes. That’s interesting in itself but, it would be even more interesting if we could gain a decent understanding of how different patients respond to various drugs. We currently have nine classes of drug but who should be given what? We’re not quite there yet. However, it is the first step towards what we call personalised medicine,” says Mikael Rydén.
Results must be confirmed
The new division proposed by the Swedish-Finnish research group will not however have any short-term effect; that is not how research works. The results must be confirmed in multiple studies and perhaps then the World Health Organisation (WHO), together with US and European organisations representing specialist diabetes doctors, will eventually sanction a change – but this will take time.
“It will be very interesting to follow this process over the coming decade,” says Mikael Rydén.
The existing division will therefore continue to apply for the foreseeable future and will also be used for the remainder of this article.
Even if diabetes has afflicted humans for thousands of years, researchers have noted an alarming change over recent decades. Diabetes in all its forms is on the rise.

“The number of new cases of type 1 diabetes per year has doubled since the mid-1980s and Sweden and Finland are global leaders in this trend. In addition, the larger group of type 2 diabetes sufferers is also rapidly increasing in size. We published data from the Swedish Prescribed Drug Register in which we compared the total number of number of people getting diabetes between 2007 and 2013, a period during which the percentage of the Swedish adult population diagnosed with diabetes increased from 5.8 to 6.8 percent. I make the figure for 2017 to be 7.8 percent, with type 2 diabetes sufferers being by far the largest group,” says Sofia Carlsson, senior lecturer and epidemiologist at Karolinska Institutet’s Institute of Environmental Medicine.
According to her calculation, over 600,000 Swedes now suffer from diabetes.
“We calculate that the lifetime risk of a Swedish person becoming diabetic is one in five,” she says.
The underlying causes of the increase in type 1 diabetes are unknown. Some researchers highlight the hygiene hypothesis, which proposes that we now live in such clean surroundings that our immune systems are underworked and begin to attack our own bodies. However, this hypothesis is as yet unproven.
The underlying causes of the increase in type 2 diabetes are more apparent. Over the past half century, major social changes have taken place that have increased the risk of developing diabetes. A number of studies have demonstrated that we exercise far less, particularly in terms of everyday exercise. Where once we walked or cycled to work, we now use public transport or take the car, we use the lift or escalator instead of the stairs, and so on.
Being overweight or obese
At the same time, food has become cheaper and access to fast, not always healthy, food has increased dramatically. Being overweight or obese reduces insulin sensitivity, or insulin resistance, increasing the risk of suffering from diabetes.
“We are built to walk a great deal, to eat relatively low-calorie food and to sleep when it gets dark, all of which have now gone out of the window,” says Mikael Rydén.
The ability to store energy when food is plentiful in order to survive periods of famine – once an evolutionary advantage – has now become a deathtrap, among other things leading to an increase in type 2 diabetes.
“We now have the opportunity to pack away calories as never before. A Mars Bar contains 200 kilocalories and one would have to stuff a lot of roots and berries to reach that level,” says Mikael Rydén.
And this change has been rapid. The past 50 years have seen immense changes to both access to food and the need to exercise.
“We have developed a society designed for maximum comfort. Portion sizes are increasing. In the 1970s, when I grew up, the largest bottle of soda available was 33 centilitres; now there are 3 litre bottles – with 10 percent sugar content,” continues Mikael Rydén.
An ancient story
The first documented descriptions of diabetes are found in Egyptian manuscripts written 3,500 years ago. The first working treatment arrived in 1922, when insulin was tested with dramatic results; a discovery that saw Frederick Banting and John Macleod awarded the Nobel Prize in Physiology or Medicine the following year.
Banting and Best, who had patented the discovery, donated the rights and production of insulin quickly escalated. As a vote of thanks, in 1991 World Diabetes Day was established on Frederick Banting’s birthday, 14 November.
Sources: Diabetes Canada and The International Diabetes Federation
THIS DEVELOPMENT IS mirrored in large parts of the world, and in some regions it has been even more rapid than here, he points out.
“In China, 8-9 percent of the population now suffer from type 2 diabetes, and that’s a country where the disease barely existed in the 1970s. However, one only need look at a photograph of Beijing in the 1970s and compare it with one from 2018; in one there will be a thousand of bicycles for each car and in the other, exactly the opposite,” he observes.
One bright spot when it comes to Sweden is that the percentage of type 2 diabetes sufferers diagnosed each year does appear to have levelled out and even shows signs of decreasing.
“That the total number of patients is still increasing is a result of longer survival times thanks to improved treatments, as well as an ageing population,” says Sofia Carlsson.
Swedes also appear to have absorbed the available information about how the risk of type 2 diabetes can be reduced. In addition to eating a Mediterranean diet – with plenty of vegetables, fish, seafood, white meat, healthy fats, fruits and berries, beans, peas and lentils – physical activity is an excellent antidote to the increased prevalence of type 2 diabetes.
And it doesn’t take a great deal. Studies have shown that a brisk half-hour walk five days a week reduces the risk of suffering type 2 diabetes by 30 percent. That the effect of such a relatively small amount of exertion can be so great is explained by the many positive effects, explains Anna Krook, professor of integrative physiology at Karolinska Institutet’s Department of Physiology and Pharmacology.

“When you train and exert your muscles, you reprogramme them. Of course, using your muscles makes you stronger but reprogramming also occurs at a molecular level, improving the ability to absorb glucose. The signalling network of the muscles becomes more sensitive, improving the response to insulin. The number of mitochondria increases, meaning that you burn fat more after exercising muscles. Muscle mass also increases after training, which in itself requires a certain amount of energy,” she says.
With regard to the question of which type of training, for example training with weights or cardio, is most beneficial for preventing diabetes and other diseases, her response is unequivocal.
“Above all, whatever training you do is the best,” she says.
Health effects of weight training
Anna Krook explains that research is less advanced into the health effects of weight training than cardio, making it hard to compare the two forms of training, although she does allow herself a qualified guess.
“If one solely looks at insulin sensitivity, in all likelihood they are roughly equally beneficial; however, cardio has a number of additional positive effects on other organs, so it might be somewhat better. At the same time, weight training can be more achievable for the elderly, and the retention of muscle mass is an extremely important parameter for avoiding fall accidents and remaining independent,” she says.
Anna Krook also points out that some studies have suggested that not everyone responds equally well to physical activity, although she believes that this is simply a matter of identifying the correct exercise.
“It may be that the right training for the right individual is key,” she says.
Currently, many patients with type 2 diabetes are prescribed physical activity by their doctor, something that large studies have shown to have an excellent effect, sometimes even better than drug treatments. The problem is that these studies are often very ambitious in scope, with physiotherapists, behavioural therapists, doctors and nurses assisting in encouraging participants to actually carry out the planned physical activities. However, when this is translated into Swedish primary healthcare, the resources are often lacking.
“In healthcare, we must prioritise the sickest individuals meaning that in practice, preventative measures fall by the wayside, even though in the long-term it may be these that offer the greatest benefits in terms of survival and quality of life,” says Mikael Rydén.

However, even if there is a clear correlation between being overweight/obese and type 2 diabetes, it is probably not that simple. Not everyone who becomes fat develops diabetes; some people appear to avoid the disease despite being just as overweight as sufferers. Why this should be is unclear, but it is something that Myriam Aouadi is attempting to ascertain. She is a researcher and leader of a research group at Karolinska Institutet’s Department of Medicine, Huddinge.
“Approximately one third of obese people have a healthy metabolism and do not develop diabetes. I am trying to understand why,” she says.
One prevalent hypothesis is that the development of type 2 diabetes is triggered by an inflammatory process, given that a number of years ago large numbers of macrophages, a type of immune cell, were discovered in the fat of sufferers.
“Over the past decade, researchers have attempted to understand what macrophages do in the fat and if they can be the underlying cause of those metabolic diseases linked to obesity,” says Myriam Aouadi.
She and her research group have developed a method for removing macrophages from the tissue, sequencing their genes and assessing what differentiates macrophages in overweight and thin individuals, both with diabetes and without. They may do this by examining animal tissue or using human tissue removed during biopsies.
“When we did this, we saw that these macrophages do not produce any more inflammatory substances, that is to say, there was no inflammatory activation of macrophages in diabetes. Therefore, something else must be happening,” she says.
Instead, they discovered significantly upregulated genes in both fat mice and fat humans. With the aid of a method developed in-house, they are able to shut down different genes in macrophages in living animals. After a number of attempts, they were able to identify a previously unknown gene involved in insulin regulation that countered the development of diabetes in mice receiving a fatty diet.
“The mice still became fat, but their blood sugar did not rise above acceptable levels and they did not have a lot of fat in their livers, leaving them metabolically healthy despite their obesity.”
Human liver cells
They have also been able to identify the same process in human liver cells. In addition, they have demonstrated that macrophages in the human liver have a natural mechanism for shutting down that specific gene.
It is too early to say exactly how this all hangs together, although Myriam Aouadi believes that they are on the track of something important.
“We believe that there are various types of macrophage that do both good and bad things to the same tissue, and we are currently attempting to map these. I believe that as yet we have only seen the tip of the iceberg and that our research will open up for an entirely new chapter on macrophages,” she explains.
If this is true, then these new findings may result in entirely new drugs and therapies.
However, today we already have a large number of treatments available. In fact, since the end of the 1990s, a steady stream of drugs have appeared primarily aimed at type 2 diabetes. There are now no less than nine classes of drug available to combat type 2 diabetes. This offers increased opportunities to identify a treatment to suit any patient, even if it does make the choice of therapy more difficult compared to 30 years ago, when only three types of drugs were available.
The primary purpose of treating elevated blood sugar levels in diabetics is to prevent negative consequences later in life. In the case of both type 1 and type 2 diabetes, this is a matter of avoiding eye, kidney and nerve damage and foot ulceration. Type 2 diabetes in particular brings with it an increased risk of death from cardiovascular disease, as patients are older and often have additional risk factors such as high blood pressure and disrupted blood fats. Many therefore see type 2 diabetes more as a cardiovascular disease, given that seven of ten patients die from some form of cardiovascular complication.
An aggressive reduction of blood sugar has been shown to have beneficial effects on damage to eyes, kidneys, nerves and feet, although the effect on cardiovascular risks in type 2 diabetes remain a matter for debate. Until now.
In clinical trials on many thousands of patients over recent years, diabetes medicines from two drug classes have been shown to reduce the risk of death from cardiovascular complications, myocardial infarction and stroke in patients with type 2 diabetes. These are the new antidiabetic agents empagliflozin (Jardiance) and canagliflozin (Inovokana), both of which belong to the SGLT2 drug class, and liraglutide (Victoza) and the newly approved semaglutid (Ozempic), both GLP-1 receptor agonists.
This has led to a higher priority for treatment of type 2 diabetes patients who also have, or have a high risk of developing, cardiovascular disease with these new drugs, in both new Swedish National Board of Health and Welfare and Medical Products Agency guidelines issued last year.
Blood-sugar-reducing tablet
First-line treatment for nearly all type 2 diabetes patients is the blood-sugar-reducing tablet metformin, which has been in use since the 1950s. However, for type 2 diabetes patients with concurrent cardiovascular disease, these SGLT2 inhibitors and GLP-1 receptor agonists have now become second-line alternatives when metformin proves insufficient. This means that a relatively large group of diabetes patients may now need to change their medication.
“Not everyone with cardiovascular disease should be transferred to these drugs. However, it should certainly be given due consideration for patients with no impediment to taking these drugs and who have many years of life to gain. This may turn out to be a fairly large group, given that 20-25 percent of all patients with type 2 diabetes are thought to either have or be at high risk of developing cardiovascular disease,” says Mikael Rydén.
This though is not something that will automatically happen. Local health centres will not contact the patients in question, but rather patients will need to take the initiative and discuss their treatment and any changes with their doctor.
“Unfortunately, as usual it will probably be the more well-read patients who benefit,” says Mikael Rydén.

When it comes to patients with type 1 diabetes, the choice of medication is not especially complicated. Patients must be prescribed insulin in various forms.
“Type 1 diabetes is caused by the failure of the body’s own insulin-producing cells, leaving one in need of substitution therapy. What we attempt to do is to as far as possible replicate the body’s own secretion of insulin.” says Jan Bolinder, professor of clinical diabetes research at Karolinska Institutet’s Department of Medicine, Huddinge.
This is achieved by using long-acting basal insulin that provides the body with the necessary base level of insulin. Fast-acting mealtime insulin is then added in the form of an injection immediately prior to eating, to deal with the rise in blood sugar levels caused by the meal.
Over the years, insulin molecules have been modified, thus refining the treatment, although it remains fundamentally the same.
Changes in the field of type 1 diabetes have primarily been on the technical side, in the form of insulin pumps and glucose sensors.
Instead of injecting insulin using a syringe or pen, a pump can be used that can be controlled by the patient. Insulin pumps have proven particularly successful for diabetic children, among other things due to their improved glucose control, avoidance of needles, simpler dosing of mealtime insulin and constant availability of insulin.
“Approximately two-thirds of all [diabetic] children and adolescents in Sweden have pumps, while the equivalent figure for type 1 diabetic adults is approximately one quarter,” says Jan Bolinder.
Checking their own blood sugar
In parallel with the development on the pump, there have also been rapid developments in terms of patients checking their own blood sugar levels. Patients have long had the ability to monitor their blood sugar with a pinprick and blood glucose meter. However, the problem is that blood sugar levels vary so much over the course of the day that individual measurements provide a fairly poor image of reality. Glucose sensors have now been developed that can be inserted beneath the skin to automatically measure glucose levels (sugar) more or less continuously.
“A continuous correct value is always available, as well as a graph of sugar checks over recent hours that shows the curve of blood sugar levels. This allows you to monitor trends; whether sugar levels are on the way up or down and perhaps are at risk of becoming dangerously low, so that one can take preventative measures,” says Jan Bolinder.
These sensors have evolved to include alarms of various kinds that can warn the user if sugar levels are too high or low, so that proactive measures can be taken. Glucose sensors have been an even greater success than insulin pumps, and in Sweden they are used by six of seven children and six of ten adults.
“The launch of a simpler and cheaper sensor system that requires active reading by the user has contributed greatly to this paradigm shift for self-monitoring. Clinical studies have also documented that the use of sensors leads to improved control of sugar levels, reduced risk for low blood sugar and, not least, an improved quality of life,” explains Jan Bolinder.
The latest development is the linking of sensors and pumps, providing a more self-contained monitoring system that functions somewhat like an artificial pancreas. Hybrid closed-loop systems are now available that can reduce the supply of insulin if sugar levels are threating to sink too low, as well as increase supply if the tendency is towards rising dangerously. The system works automatically overnight and between meals. However, the patient still needs to manually dose mealtime insulin using the pump.

Completely automatic systems that can also handle mealtime insulin have existed for a number of years and are currently undergoing clinical trials, but as yet these are not commercially available. The better these systems become, the more closely treatment will resemble the natural secretion of insulin from the pancreas; all for the purpose of preventing negative consequences later in life.
“In the short term, glucose control and quality of life will be improved while, in the long term, improved blood sugar control will reduce the risk of subsequent complications,” says Jan Bolinder.
One form of diabetes that seldom receives much attention is the type 1 variant latent autoimmune diabetes of adults (LADA), this despite the fact that the size of this group of patients is estimated to be of the same order as for type 1 diabetes. LADA is often confused with type 2 diabetes as it presents during adulthood and patients are often overweight. However, because the immune system kills insulin producing cells, the majority of these patients will sooner or later require insulin treatment. The disease seems to be a mixture of type 1 and type 2 diabetes.
“If type 1 diabetes runs in your family, the risk of developing LADA increases sixfold, while type 2 diabetes in the family ‘only’ doubles the risk compared to someone with no history of diabetes in the family. However, the link to lifestyle is still fairly close to type 2 diabetes. It is the factors that affect insulin resistance – such as being overweight, a sedentary lifestyle and smoking – that seem to trigger LADA,” explains Sofia Carlsson.
Studies LADA patients
She is leader of the ESTRID study, a project that studies LADA patients from two Swedish patient registers and identifies risk factors for developing LADA, which she compares with patients with type 2 diabetes and a healthy control group.
One factor that sticks out in her findings is coffee. Coffee clearly offers some protection from type 2 diabetes, while it also seems to increase the risk of developing LADA.
“We have identified two factors that appear to affect autoimmunity: oily fish and coffee. That oily fish reduces the risk is not particularly controversial, similar results have been demonstrated for type 1 diabetes in children, but for coffee I feel that we need further studies of other patient groups before we can say anything with certainty,” she says.
Sofia Carlsson will soon have 10 years of data on LADA patients in her database and she and her research group are currently preparing a follow-up to find out which treatments they are receiving and how they are progressing. Which treatment is best for LADA patients is still not entirely clear.
“We know that they have much better blood pressure, blood fats and are less overweight than type 2 patients, but they have just as high a risk of dying prematurely and contracting cardiovascular disease. This appears to be because they have poorer glucose control. In which case, one might think that they should be receiving better treatment,” says Sofia Carlsson.
She therefore hopes to be able to contribute new knowledge on how treatment can be improved. Diabetes has existed for thousands of years, but we still do not know the basic cause of the diseases. Despite this, treatments have improved significantly over recent years. It may soon be possible to redraw the entire map of diabetes once again, if the Swedish-Finnish proposal for a new division wins favour. And then, Swedish patients and researchers will very much be participating in influencing the future of diabetes patients globally.
Text: Fredrik Hedlund
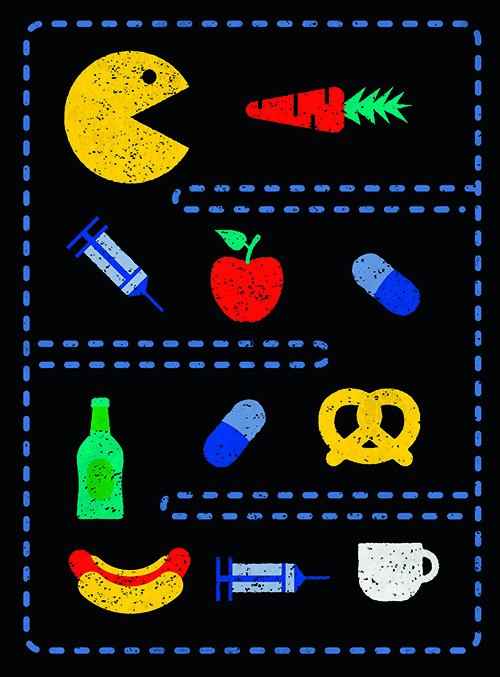
Illustrations: Jens Magnusson
First published in Swedish in Medicinsk Vetenskap No 2/2018
Different diseases
Elevated blood sugar is the common denominator for all forms of diabetes. However, the reasons for this elevation, why it occurs, prognoses and treatments vary from one form of the disease to the next. The pie chart below shows the approximate division of the various forms of diabetes.
Type 2 diabetes. In all likelihood, a number of different diseases fall under this designation, with different causes and prognoses. Normally presents in adulthood, with occurrences increasing with age. It is estimated that approximately 500,000 people in Sweden have type 2 diabetes, approximately 20 percent of whom manage their condition without prescribed drugs using only diet and exercise treatments. Treatment: Diet and exercise, diabetes drugs – primarily metformin.
Type 1 diabetes. An autoimmune disease in which the body’s immune system attacks insulin-producing cells in the pancreas. Normally presents in childhood or adolescence. There are estimated to be approximately 45,000 people in Sweden with type 1 diabetes. Treatment: Insulin in various forms.
LADA. Latent autoimmune diabetes in adults. Like type 1 diabetes, this is an autoimmune disease, but like type 2 it presents in adulthood and often affects overweight patients. The disease runs a slower course than type 1 diabetes. There are estimated to be approximately 30,000 people in Sweden with LADA. Treatment: Diet and exercise, diabetes drugs – primarily metformin or insulin. It remains unclear which treatment is most effective.
Secondary diabetes. A diabetes disease stemming from damage to the pancreas, for example as a result of inflammation, surgery, cancer or gall stones. There are estimated to be approximately 7,500 people in Sweden with secondary diabetes. Treatment: Depends on the damage, but generally insulin as for type 1.
MODY. Maturity onset diabetes in youth. A group of 13 hereditary conditions caused by mutations in a dominant gene. The disease is common in some families and affects both sons and daughters. Often confused with type 1 or type 2. There are estimated to be approximately 6,000 people in Sweden with MODY. Treatment: Varies depending on the type of mutation.
Gestational diabetes. Temporary elevated blood sugar levels due to an increased requirement for insulin during pregnancy. Up to 4 percent of all pregnant women are affected. Blood sugar levels will generally return to normal after the birth. Treatment: Diet and exercise, metformin or insulin may be administered.
Sources: Swedish Prescribed Drugs Register, ANDIS Register, Swedish Medical Products Agency, Sofia Carlsson, Mikael Rydén.
