Spotlight on ALS – hope in sight for dreaded disease
In a short period of time, knowledge regarding the neuromuscular disease ALS has increased dramatically. Now, researchers and doctors have their hopes set on new treatments being developed, and for the first time there is now talk of being able to stop the disease within the foreseeable future.
Text: Fredrik Hedlund, first published in Swedish in Medicinsk Vetenskap No 2/2019.
ALS, or amyotrophic lateral sclerosis, is a very rare but deadly motor neuron disease that causes the nerves controlling the muscles, i.e. the motor neurons, to break down and die. The sufferer gradually loses control of their muscles, followed after some time by paralysis, and eventually by death.
The progression of the disease is often fairly rapid, and patients only survive for two to five years on average following diagnosis, but there are very large variations between individual patients. The Swedish journalist and news anchor Ulla-Carin Lindquist died from ALS in 2004, at 50 years old, after being diagnosed only a year prior. In contrast, the famous theoretical physicist and mathematics professor Stephen Hawking lived 55 years after being diagnosed at the age of 21. He died last year at the age of 76.
The large disparities between different patients not only relate to how rapidly the disease progresses, but also to when it first presents.
“I remember a patient I met at an ALS conference I attended in the US as a researcher in the early 2000s. He was in his 60s and had recently started exhibiting symptoms of the disease. He told me about his brother who had died from ALS before turning 30. They both carried the same mutation in the gene SOD1, which causes ALS. This shows that there can be great disparity between individuals, even within the same family,” says Eva Hedlund, ALS researcher, research group leader and docent at the Department of Neuroscience at Karolinska Institutet.
It has been clear for some time that there is a genetic component to ALS, and doctors classify the disease into the categories of familial ALS, where several people in the family have been diagnosed, and sporadic ALS, where there is no such family association. However, the clinical applicability of this classification is limited as the disease can behave in different ways, even within the same family. Other than possible onset at very different ages, it can also start in completely different muscle groups and also skip one or two generations.
Not simple genetics
However, developments within genetic research have meant that knowledge on the correlations has grown and become increasingly clear. But this is not simple genetics. So far, the researchers have been able to describe mutations in 36 different genes in the hereditary forms of ALS, and at least a further nine genes can be linked to ALS but they have not yet been identified. The new knowledge also shows the difficulty of the classification system. Patients have, for example, been found who have familial ALS but completely lack any of the identified ALS genes, as well as patients with sporadic ALS with classic mutations.
It is said today that between 10 and 20 per cent of the ALS patients have an identified genetic cause for the disease, while the cause is yet unknown for the remaining 80 to 90 per cent.
The most common ALS gene is called C9ORF72 and was discovered as recently as 2011. The mutation in this gene means that a short DNA sequence is repeated hundreds or thousands of times, which makes the gene unstable and leads to the formation of a toxic protein that poisons the motor neuron.
The second most common ALS gene was discovered in 1993. It is called SOD1 and has been significantly more researched. In this gene, the researchers have thus far found more than 200 different mutations that increase the risk of developing ALS. The different mutations likely cause different disease progressions, but the correlation is complicated since genetics is not always enough to explain the onset of the disease.

“Mutations in the SOD1 gene are dominant so you only need to inherit the disease-inducing mutation from one parent in order to get the disease. But some individuals can carry an SOD1
mutation their whole life without being sick, or they succumb late in life. Since this is the case, there must ultimately be something in their environment or lifestyle that has an effect. We are thus dealing with a combination of genetic factors triggered by environmental factors,” says Caroline Ingre, specialist and head of ALS activities at Karolinska University Hospital, as well as group leader for the ALS research at the Department of Clinical Neuroscience at Karolinska Institutet.
Researchers are therefore mapping both genetics and environmental factors trying to understand how they are related, and the knowledge is rapidly growing. For example, a few years ago researchers were able to prove that the mutation in the gene C9ORF72 also increases the risk of suffering frontotemporal dementia, and just recently it was also linked to an increased risk of mental illness and psychosis in the family. This prompted a serious reappraisal.
“Previously, when we asked patients if anyone else in their family had suffered from ALS, and if the answer was no, it was classified as sporadic ALS. But maybe it turns out that their mother, grandmother and great grandfather all suffered from schizophrenia. Then perhaps it wasn’t sporadic ALS at all, but familial, and we just didn’t see the connection before,” says Caroline Ingre.
Genetic investigations
She says that the ALS centre at Karolinska University Hospital offers genetic investigations, including the patient’s siblings and parents, in order to better map and understand the correlation.
But what are the environmental factors that can trigger ALS? The epidemiologist Fang Fang, a docent at the Department of Medical Epidemiology and Biostatistics at Karolinska Institutet, is trying to find evidence of which factors are important.

Age and family history are uncontroversial risk factors. The older you are, the higher the risk of suffering illness, and the family history is of course the source of the genetics, but other things like your lifestyle growing up also seem to play a part, according to Fang Fang. Men are also at a higher risk, as are smokers.
“These are factors where we are certain that they are risk factors for ALS,” she says.
Other risk factors that have also been seen in a number of epidemiological studies, but which are less established, include physical activity, where light physical activity appears to protect against ALS, while hard physical activity instead increases the risk. In a highly noted study, Fang Fang has previously been able to show that elite skiers in the race Vasaloppet had a higher risk of ALS, while the recreational skiers had a lower than average risk. The reason for this remains unknown however.
High blood lipids have also been seen in several ALS studies, with scattered results, but there is now sufficient evidence to establish a correlation, says Fang Fang.
Risk factors
“Over time, these risk factors are becoming increasingly clear. I think that we can now say that high levels of bad cholesterol, especially LDL, constitute a risk factor for ALS,” she says.
The same is true for low BMI and a low level of education, which also appear to be clear risk factors. Then there are other risk factors which have been presented, such as exposure to various metals, as well as protective factors such as high consumption of alcohol and coffee which have not yet been sufficiently confirmed.
“The evidence base is fairly weak for these factors. So we probably shouldn’t draw any far-reaching conclusions,” says Fang Fang.
There are thus a handful of risk factors, with some being possible to influence and others not, which increase the risk of ALS. And then there is a group of factors where further research is necessary in order to really say how important they are.
A good question is what to do in order to minimise the risk. But for the normal population there is no reason to think like that, according to Fang Fang.
“Luckily, ALS is a rare disease. This means that you do not need to worry about reducing the risk. You can of course try to lower your bad cholesterol, but you should do that to reduce the risk of cardiovascular disease and cancer, not ALS. If, on the other hand, you have a family history of ALS, that’s a slightly different matter,” she says.
Large individual variation
As previously mentioned there are large individual variations in the progression of the disease, but the reason for this is unknown.
“We have an ALS population where the vast majority will die within three years, just as all the studies say. But we are seeing that 10–15 per cent have a long life, like Stephen Hawking, and 10–15 per cent live much shorter than three years. So already within this group there is significant individual variation, and we haven’t even started talking about genes,” says Caroline Ingre.

She says that the patients go through genetic testing, and no correlation has been found with the disease progression. As a treating physician she is interested in being able to predict how quickly an individual patient’s disease will progress, in order to adapt the measures she takes.
“For me, it is very much a matter of care. We are doing research on these patients in order to predict their disease progression. Patients whose illness is progressing at different speeds will most likely need different forms of treatment in the future, but at the moment it is more a matter of trying to adapt the care to the patients’ needs. Much of my research is about identifying biomarkers for early diagnostics and finding prognostic biomarkers in order to determine which patients will have a slow progression and who will have a rapid one,” she says.
And she has now managed to develop a package of various biomarkers based on brain imaging, PET scans, genetic analysis, and several different biomarkers from spinal fluid and blood samples.
“When you have ten of these biomarkers, you can form a good idea of the patient’s future. I can for example say to some of my patients that now that I have met with you a few times, and considering these biomarkers, it is unlikely that this disease will progress rapidly,” says Caroline Ingre.
A primary-care rehab team
This also means that she can adapt the care so that it is better suited to each individual patient.
“For patients whose disease is progressing slowly, you can connect them with a primary care rehab team, they can go on rehabilitation trips and they can exercise more. For those with a more rapid disease progression, it is perhaps better to have them work closer with us at the specialist centre and connect them with palliative care at home in order to support their families and children,” she says.
She says that the health service has been treating all patients the same so far, which has not been effective.
“You meet with them every three months until they die. It’s terribly ineffective considering the patient’s needs. We are working hard to change this,” she says.
She gives the example of one of her current patients, whose disease is progressing very quickly.
“I have told the patient’s family members that I would like them to come along for every visit, because otherwise they won’t be able to keep up with the disease. This has been absolutely crucial for allowing this family to deal with the disease. In just one or two months, the patient has lost a great deal of function. But during that time I have seen the patient much more often, my nurses have been in close contact, and the patient’s entire family have been able to be here, so we have still managed to stay one step ahead. Even if there is nothing we can do to stop the disease, we can definately frame it and provide support in a much better way,” she says.
Because although knowledge about ALS has increased greatly over the last decade, there are still no new drugs. The only available drug, riluzol (Rilutek), was manufactured in the 1990s and it slows the disease progression somewhat. Clinical studies have indicated an increased survival period of three months, but Caroline Ingre argues that it provides more than that.
“We divide the ALS progression into five stages, and Rilutek slows the progression in each stage; you see large differences in survival time, so it gives a greater effect than three months,” she says.
But several new treatments are currently being developed, which could change the situation a great deal. Closest to clinical application is the drug edaravon (Radicava), which has already been approved in the US and Japan.
“We hope that it will be approved and made available for treatment in Sweden by the autumn,” says Caroline Ingre.
Only one subset of patients
However, only one subset of patients in the clinical trial experienced an effect from the treatment; those who had been ill for a period of less than 18 months and who still had a good breathing capacity.
“We will be able to offer these patients the new treatment, while the patient groups that saw no effect in the study will not be getting it. One of the reasons being that it is administered intravenously every day, which has a fairly big impact on the patient’s quality of life,” says Caroline Ingre.
The new treatment also highlights another central aspect, which is that it is important to start treatment as early as possible. ALS breaks down the motor neuron, which then causes the muscles to atrophy. The researchers’ primary goal is to find a treatment that stops this process.
“All indications point to it being necessary to continuously make an earlier diagnosis, which we can only do through increased awareness,” says Caroline Ingres.
Because although there are still gaps in our understanding and today’s drugs have only a limited effect, one major issue is that it often takes approximately one year from the onset of symptoms until the patient sees a neurologist and is actually diagnosed.
“We are currently conducting a study to see if it is possible to get the same results in blood from a biomarker that we now take from the spinal fluid. If that were possible, the health service can take a blood sample upon the smallest suspicion, and if they get an elevated result, they can send the patients straight to us,” says Caroline Ingre.
As much as it would improve the present situation, it is a way to prepare for the future, when Caroline Ingre and other doctors will be able to do more than they can today. Because both clinicians and researchers in the ALS field have a very positive view of the future. A review of the current research situation shows that there are some 20 new treatments on the way, the first of which could start being used clinically within just a few years.
These include everything from brand new substances to different types of gene therapy – those where the patient’s genes are modulated, and those where mutations can be “turned off” without altering the patient’s genes, i.e. antisense therapy. There are also a number of existing drugs being tested for the first time for ALS, and which could be approved quickly if they turn out to be effective.
Antisense therapy has yielded very promising results in animal models, and the hope is that they will be equally effective in humans – something that is currently being tested in clinical trials. However, antisense therapy will only be possible to use on those patients whose genetic mutation is known. It may also require separate treatments and approvals for each type of mutation. For this reason, there is a need for more general treatments. Something that Eva Hedlund, who conducts basic research in neurology, has focused on in her research.
Different motor neuron groups
With ALS, an increasing number of motor neurons start to break down and die, but not all. The disease can start in different motor neuron groups and spread over time, but the motor neurons that control the eye muscles, the oculomotor neurons, keep functioning until the end. Eva Hedlund is interested in why this is the case, and whether this fact can be used in some way.
“The oculomotor neurons are incredibly resilient, and this is something that is used clinically for ALS patients who are completely paralysed, enabling them to communicate with the people around them thanks to computerised aids. We have studied these motor neurons carefully and tested whether we could transfer any of their properties to sensitive motor neurons in order to make them more resilient,” she says.
Which they did. She and her research group found high concentrations of two growth factors in the nerve cells of the eye muscles. These growth factors are known to protect the motor neurons, but it was previously unknown that they were so abundant here.
“If we add the growth factors to human spinal motor neurons, which we grow from stem cells in the lab, they do much better in an ALS-like environment; they don’t degenerate nearly as quickly. Using gene therapy, we have also been able to increase the resilience of sensitive motor neurons in ALS mice, which allowed the animals to live longer,” says Eva Hedlund.
However, she does think that a truly effective therapy needs to target several different mechanisms in the cell. For this reason, she and her team have continued to research the oculomotor neurons. They have developed new techniques to study both what happens in the cell body of the motor neurons and in their long extensions, the axons, when they are exposed to mutations that cause ALS, and they have found new molecular pathways that could be used.
She thinks it is looking promising, but cannot say anything else at this early stage. In any case, the plan is to arrive at something that can act as good protection for sensitive motor neurons, regardless of which mutation the patient has, as well as in the many cases where there is a clear genetic mutation linked to the disease.

Another way of attacking the disease comes from Oscar Fernandez-Capetillo, professor of cancer therapy, who recently made a career change to become an ALS researcher at the Department of Medical Biochemistry and Biophysics at Karolinska Institutet. He has recently published an article in the scientific journal Cell Chemical Biology on a new way of screening for ALS drugs.
Using advanced microscopes and robots, he is able to simultaneously analyse the effect of approximately 400 different substances on cells being subjected to the toxic protein created from the mutation of the most common ALS gene, C9ORF72. The effects are photographed and computers analyse the images to identify the substances that protect the cells from the toxin.
“In that way, we are able in a very short time to study the effects of tens of thousands of substances on human cells,” says Oscar Fernandez-Capetillo.
Finding useful substances
In the published article, he presents the results from testing of around 5,000 substances, where they found three that were actually able to protect the cells. But Oscar Fernandez-Capetillo does not make too big of a deal of this trial.
“This was my first trial at Karolinska Institutet. So for a screening lab, this was, I wouldn’t call it a beta test, but we were checking that we had put the machines together right. One of the three substances that we identified using our method, we later discovered was already involved in clinical trials for ALS, so that proved the method effective for finding useful substances. That reassured us, since it showed that we are on the right track,” he says.
Even if the trial was specifically targeted to cells from patients with a mutation in the C9ORF72 gene, Oscar Fernandez-Capetillo believes it may have an impact for other patients as well.
“With the exception of the mutations in SOD1, the rest of the mutations appear to affect the motor neurons in a similar way, by regulating our RNA. This is good news for the patients. It means there is hope of finding a solution that can work for many patients,” he says.
The next step will be to use the method to screen a significantly higher number of substances, in order to find better candidates. Considering that the current treatment has led to an increased survival period of three months, Oscar Fernandez-Capetillo is setting his sights high.
“Our long-term goal is to find brand new substances that can have a real effect on the disease. For it to be significant, any new substance must provide years of extended life. If it doesn’t, I wouldn’t consider it a medicine,” he says.
Oscar Fernandez-Capetillo also believes that finding new treatments can be a relatively quick process, but he will not say how quick.
“For a long time, we only had indirect evidence, which was rather indistinct. Now, we know more about what the problem is. If you combine this with the amazing developments in the technology being used to develop drugs, I think it is only a matter of time until we have a good ALS treatment,” he says.
For most of today’s ALS patients, however, the treatment that Oscar Fernandez-Capetillo envisions will most likely come too late. He admits that this is a hard pill to swallow, but he still has one soothing thought that might give today’s sufferers some consolation.
“Hopefully their children will never have to go through what they have gone through. I feel very optimistic that there will be effective treatments for the next generation,” he says.
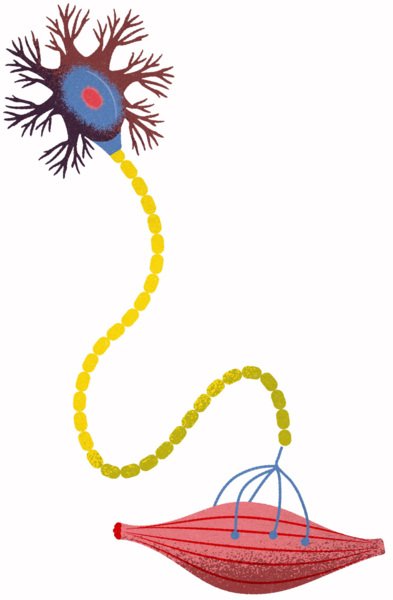
ALS in short
Amyotrophic lateral sclerosis. ALS is a lethal neurological disease that causes the nerve signals to the muscles to gradually deteriorate.
The cell body. This is the core where many processes can be disrupted in the case of ALS.
Dendritic cells. They receive messages from the brain or from another motor neuron.
Axons. Transfer the message to other motor neurons or the muscle.
Motor neuron. The nerve cells that control the muscles are called motor neurons. The consist of three main parts: the cell body, dendritic cells, and axons. In the case of ALS, there may be something wrong with all three.
Muscle atrophy. When the signals from the motor neurons are interrupted, the muscles gradually deteriorate and their function ceases.
The patient dies. Most often, the patient’s life is ended when the respiratory muscles give up and they stop breathing.
