Multiple sclerosis: A newly interpreted disease
Intensive research has led to that much of the previous approach to multiple sclerosis has been revalued. This applies to both the process and how the disease should be treated. Scientists also know much more about risk and protective factors, knowledge that can be used preventively but also to understand more about the mechanisms behind the disease.
This article was first published the magazine "Medicinsk Vetenskap" No 4, 2016.
Knowledge regarding the neurological disease multiple sclerosis, MS, has positively exploded in the last 20 years. Prior to this, MS was something that doctors could only diagnose and provide some symptom relief for, but now there is a plethora of drugs that can slow the course of the disease.
“I have been involved in MS research for 30 years. The first year I went to an MS conference, 75 people turned up, whereas this year 10,000 neurologists were in attendance. It has been an incredible journey, especially during the last 20 years,” says Tomas Olsson, Professor of Clinical Neuroscience at Karolinska Institutet.
The first disease-modifying therapy was approved in 1995, but it is really in the last ten years that big developments have happened. Since 2006, seven new drugs for MS have been approved by the authorities in Europe. At the same time, knowledge of the underlying factors relating to the disease has increased dramatically, both on the genetic factors involved and the lifestyle factors that increase the risk of MS. And researchers at Karolinska Institutet have greatly contributed to the development of this knowledge.
Thus far, over 200 genes have been identified whose variants have greater or lesser significance in terms of the risk of developing MS. The most important are the genes in the so-called HLA region, which is involved in the manifestation of “human leukocyte antigen”, antigen-presenting molecules found on the cell surface. The HLA region is found on chromosome 6.
“There are a number of important genes, and the most important gene variant goes by the simplified name HLA DRB15. If you have this gene variant, the risk of getting MS increases by two and a half to four times,” says Ingrid Kockum, Professor of Genetic Epidemiology specialising in Multiple sclerosis, at Karolinska Institutet.
The other gene variants contribute to a much lesser degree in terms of risk increase; between five and twenty per cent, researchers estimate.
“This is a much lower risk when viewed individually, but together it becomes significant,” says Ingrid Kockum.
The fact that so many genes are involved means that it becomes a complicated pattern with regard to how large a role the individual genes actually play; in many cases, it is very small, according to Ingrid Kockum.
“Many of us are walking around with a whole bunch of MS risk variants but don’t get MS,” she says.
This is also why the heritability of the disease is not so pronounced. Children of a parent with MS admittedly are ten times more likely to get the disease, but as the baseline risk is only two per thousand, this means that only one out of fifty children of a parent with MS inherits the disease.
“If there are a wide range of genetic factors that influence the risk level, it’s not so likely for someone to have them all. It's not a monogenic disease, such as cystic fibrosis, where mutation in a gene leads to disease emergence,” says Ingrid Kockum.
Many genes are involved
The fact that so many genes are involved will also make the interpretation of individual sets of genes difficult, but this is not the purpose of the mapping either.
“We will most likely not be able to predict who will or will not develop MS. However, I believe that genetic knowledge is very important in order to understand the biological processes involved in the disease. But then it is not enough to find where the mutation is located. We also need to understand what it does, what affect it has,” she says.
And in this respect, the researchers are still on the starting blocks. What they will say is that very many of the interesting genes they have found are involved in the immune system. This is something that further strengthens the prevailing hypothesis that MS is an autoimmune disease.

With a deeper understanding of the biological processes involved in MS, it will be easier to find new targets for treatment. It is not certain that it is necessary to understand everything, suggests Ingrid Kockum.
“I think that many different things have to go wrong in order to get MS, and perhaps it is enough if we can stop some of these to prevent the disease from emerging or to cure it,” she says.
Although researchers have now found more than 200 gene variants that affect the risk of MS, they have not found all of them.
“We can now explain about 30 per cent of the heritability with these upwards of 200 gene variants. And this is partly because we have not identified all the genes, but it could also be because we have wrongly estimated the risk. The issue is that we have assumed that each gene is acting by itself, and it is quite obvious that this is not the case. There are combinations of different genes and combinations of environmental factors that when combined lead to a much higher risk when compared with the risk entailed by each one individually,” says Ingrid Kockum.
The research on environmental factors – environment and lifestyle – has also resulted in a significant increase in knowledge over the past decade. Smoking, low levels of vitamin D and obesity are three factors that we have observed contribute to an increased risk of MS. Getting glandular fever in adolescence rather than as a child also seems to increase the risk, as does shift work and organic solvents.
What actually happens when these factors increase the risk is something we do not know for sure, but there are hypotheses. It is clear in any case that you have to be exposed to the risk factors before the disease onset, and since MS manifests fairly early on, there is a rather short period of life involved.
“Many of the risk factors that we have identified, such as low vitamin D, shift work and high BMI, seem to act from puberty until the age of twenty; then they have less effect. It appears that you run the risk of MS in your late teens depending on genetic predisposition and trigger factors. The same applies to the Epstein-Barr virus (glandular fever). If you get it in adolescence, it's worse than if you get it as a child,” says Tomas Olsson.

Among the lifestyle factors, there is one that stands out as particularly risky, and that is smoking. Anna Karin Hedström is a postdoctoral researcher at Karolinska Institutet and she wrote her thesis in 2015 on tobacco and its effects on the development of MS.
“We have looked at smoking in the context of the various forms of MS and we can clearly see that smoking is not limited to a window in youth. If you look at smoking before the disease onset you can see that it has as much impact even if you started smoking later in life. Smoking seems to be as influential a risk factor at any time,” she says.
Continue to smoke
In her dissertation, Anna Karin Hedström could also show that smoking had a clear dose-response relationship, meaning that the more you smoke, the greater the risk increase. In addition, the patients who continue to smoke have a worse prognosis than those who quit.
“Smoking is not only a risk factor for MS, it also has a negative impact on the entire course of the disease,” she says.
Anna Karin Hedström could also show that the risks of smoking also apply to passive smoking.
“If you look at those who have never smoked, you can identify a clear increase in risk for those exposed to passive smoking. What can also be seen here is that the longer you have been exposed to passive smoking, the greater the risk increases,” she says.
But it is not the nicotine in cigarettes that is the culprit as you might expect; in fact, it is probably the opposite.
“In the beginning we isolated the group of moist snuff users, and then we saw that they had a reduced risk of MS. Over the years we have amassed material and repeated the study, and we can see very clearly that moist snuff users have a protection. There are many indications that it is the nicotine that is the protective element as we know that nicotine has an anti-inflammatory effect,” she says.
In the case of moist snuff there is also a dose-response relationship entailing that the more you use moist snuff, the greater the decrease in risk. It is even noted that smokers who also use moist snuff run a lower risk than those who only smoke.
“It is therefore the moist snuff that reduces the risk,” she says.
Anna Karin Hedström has a theory about how it could be connected.
“Our hypothesis is that it is a lung irritation from the smoke that could trigger an autoimmune reaction. If autoimmune cells are activated in the lungs, they automatically take on properties which enable them to enter the brain,” she says.
This would also sync up well with one of her latest findings, that organic solvents seem to have a similar risk profile as smoking, including the gene-environment interaction with the HLA DRB15 gene. This is something she intends to pursue further.
Aside from moist snuff, Anna Karin Hedström and her research colleagues have also found other protective factors which are, to a layperson, about as unexpected as moist snuff. What about the protective factors coffee and alcohol? In quite high quantities too.
“When it comes to coffee, there is no real effect until you get up to four or five cups a day. And with alcohol, you also need to reach a certain level of consumption before effects are noted,” she says.
Need to be verified
She points out, however, that the findings regarding coffee are brand new and need to be verified in several studies in order to assured. Admittedly she compared two very different groups of patients, one in Sweden and one in the US, and saw the same thing in both – the large consumers ran a lower risk.
As lifestyle factors affect the risk of developing MS, an individual can personally alter their risk level, but Anna Karin Hedström stresses that MS is a fairly rare disease and that most people will never contract it. However, given that the disease is partly hereditary, people with MS in the family may need to think about reducing their risk, or rather not increasing it.
“In which case you should definitely not start smoking and you should also ensure that your child is not exposed to passive smoking. You should also try to avoid your children becoming obese as child and adolescent obesity is a significant risk factor,” she says.
Spending time outdoors is also important since sunlight releases vitamin D in the body. The protective factors are of course a bit trickier to manage with prevention in mind, she admits. They have more of an academic interest.
“Naturally, you can’t recommend that children start using moist snuff and drinking coffee or alcohol, but the findings can help us understand the mechanisms behind the disease,” she says.
The fact that a lot of new knowledge regarding risk factors for MS is currently emerging, and that Sweden in is many cases a world leader with regard to this knowledge building, is in large part due to the Swedish MS Registry. The registry started in 2000 and now contains approximately 17,500 MS patients, which is over 80 per cent of all patients in Sweden. That makes it one of the world's most comprehensive MS registries.

One of the reasons why it has become so successful is that the registry is not an administrative burden for the attending physicians, but rather a useful tool. Therefore almost all MS doctors in Sweden contribute information to the registry.
“When a doctor is going to meet a patient they need to update themselves, and electronic medical records can often be difficult to browse through. In the MS Registry you can just press a button and you get the whole patient history on one screen. Moreover, by pressing another button you can see the patient in question compared with all other patients in the registry who have had the disease as long. You can then get an idea of whether the patient is where they should be, purely from a treatment perspective,” says Jan Hillert, Professor of Neurology at Karolinska Institutet and registry manager for the MS Registry.
The registry also enables research that cannot otherwise be pursued and which therefore complements the clinical studies that must be done before a drug can be approved.
“There is a lot that we can’t study in clinical trials. If we want to know whether these drugs are safe and effective over a 10-20-year period, we can’t do a clinical study. It would be unethical and is just not an option. This was one of the reasons why we produced this registry; we wanted to know what the long-term effects were,” says Jan Hillert.
In addition, the registry contains the majority of all patients and is thus more representative of the actual treatment, while the patients in clinical trials are always a narrower sample of patients.
Jan Hillert says that he initially researched the genetics behind MS, but that he has gradually crossed over to epidemiological research using data from the MS Registry.
“In Sweden as a whole, we have published about 120 scientific reports from the registry to date. That’s quite a lot,” he says.
Since Jan Hillert and his colleagues were interested in genetics from the beginning, they also did something very prudent.
“We have collected DNA samples from as many patients as we could. This means that we now have DNA samples from up to 12,000 of our patients. Because we have the registry, we can now also study gene importance for clinical parameters over time. We have also asked the patients about their lifestyle. Therefore, we can study both genes and environment, not only in terms of risk but also with regard to how the disease develops. This is something that is completely unique,” says Jan Hillert.
Both genetics and environmental factors
The MS researchers at Karolinska Institutet are actually the only researchers in the world who have from an early stage focused on both genetics and environmental factors for MS. All the others specialised in either one or the other, which now seems unwise as it appears there are many gene-environment interactions. Many research groups are now trying to supplement their profile, but the Swedish researchers are fifteen years ahead of the pack.

This is also thanks to the new knowledge that the researchers have established, the conclusion that the course of the disease was most likely misunderstood previously. Doctors have always understood the initial relapsing form to be a milder prelude to the more active, progressive phase that comes about 20 years after the onset of symptoms, when the physical functions begin to deteriorate more and more. Now we are starting to understand that in all likelihood it is just the opposite.
“When we look at markers for ongoing nerve damage we can see a very clear age correlation; it is highest among younger patients and then it drops. Many patients in the progressive phase have no specific ongoing nerve damage at all. The progressive phase is therefore not nearly as active as previously thought,” says Fredrik Piehl, Professor of Neurology at Karolinska Institutet.
He ascertains that the increasing loss of function that one sees in the progressive phase is probably mostly related to natural ageing and can be explained by the inflammation that has been going on for twenty years, already breaking down the reserve capacity that existed in the nervous system.
“It's a faster nerve-damaging process early on in the course of the disease that is not noticed, and which is insidious. A young individual has a high resistance to this and can potentially lose half of the nerve fibres running from the cerebral cortex to the spinal cord without displaying permanent symptoms. The problem is that this reserve is something you need when you get older, but then you’ve kind of missed the train,” he says.
His view is also supported by the fact that the newer immunological drugs that have been developed in the past decade clearly have better efficacy in younger patients compared with older patients. But these are fairly new insights and the current guidelines for MS treatment still indicate that one should start with milder treatments that have fewer side effects. This is something that Fredrik Piehl believes is a mistake.
“The entire process of MS treatment so far has focused on the wrong things. Often it’s the case that you treat patients who have an increasing degree of neurological disability in their later years with more effective, but potentially more dangerous therapies. We under-treat patients in the early stage and over-treat to some extent later on during the course of the disease. The biggest problem, however, is the under-treatment of younger patients,” he says.
National guidelines for MS
That being said, national guidelines for MS are currently being prepared for the first time by the Swedish National Board of Health and Welfare. They will be presented in December 2016.
One problem with an early, aggressive treatment is however that some highly effective drugs are associated with the risk of serious side effects. A good example of this is the treatment that is considered to have the best effect, natalizumab (Tysabri), which can cause progressive multifocal leukoencephalopathy, PML – a rare and at worst deadly viral infection.
More than half of the Swedish population carry the JC virus, which causes PML, something that is normally not a problem. But the immunosuppressive drug natalizumab increases the risk of an outbreak and several deaths have occurred, even in Sweden. Among those not infected by the JC virus, the risk of PML is low, but virus-free individuals can become infected, which means that everyone who is treated with the agent must be tested for the virus twice a year. Many patients must stop treatment over time and it causes an unpleasant “rebound” effect where the disease can flare up dramatically and lead to permanent loss of function.
However, last spring Fredrik Piehl and research colleagues in Göteborg and Umeå published an observational study in which they had looked at all patients in the MS Registry who had stopped taking natalizumab and started with either fingolimod (Gilenya) or rituximab (Mabthera). The latter treatment is approved for the treatment of, for example, lymphoma and rheumatoid arthritis, but not for MS, but has begun to be used by MS doctors outside of its approved indication, something that can be done within the scope of the doctor's responsibility in that doctors in Sweden have free right to prescribe medication.
It was revealed that a year and a half after the switch, fewer than two out of a hundred patients who had switched to rituximab suffered a relapse while ten times the number who had switched to fingolimod had succumbed to such. This is something that has already affected the prescription of treatments.
“If it is now working so well on individuals with the JC virus, then it should have an equally positive effect on those who don't carry the virus. This has resulted in a gradual increase in the use of rituximab in more and more patients who have high inflammatory activity,” says Fredrik Piehl.
He has continued to study the effects, and at the European MS Conference in September this year he was able to present new data on several thousand patients from the MS Registry, where the outcome for those who were prescribed rituximab was better than for those who received the other two treatments.
“I think we now have enough evidence to conclude that rituximab has a comparable effect to natalizumab, but where the risk of PML is very small. This we know from the treatment of rheumatism where a lot of treatment data is available,” says Fredrik Piehl.
An infusion every six months
In addition, treatment with rituximab is less cumbersome, indicates Fredrik Piehl, as it is given as an infusion every six months. Aside from this, patients do not need to think about their medication. And finally, the treatment is much cheaper than any other MS treatment. Compared with fingolimod and natalizumab, which cost around SEK 200,000 per year and patient, rituximab costs SEK 25,000 per year per patient.
Overall, everything seems to be close to perfect. After 200 years, a treatment has been found that is effective, safe and easy for the patients to take. All this, and at a very reasonable cost to health care.
However, there is one problem. Rituximab’s patent has expired and the company behind it has stopped the costly clinical development aimed at getting it approved for MS. Instead, they are developing a new, patentable drug with the same mechanism and similar effect – ocrelizumab – which, however, is not yet approved. But what happens when/if it does get approved?
“Will the pharmaceutical company then be able to force Swedish health care to switch treatment, even though the experience of ocrelizumab, and therein the degree of safety, is worse? This question is hard to answer,” says Fredrik Piehl.
It is clear, however, that the pharmaceutical industry is concerned about the developments they see in Sweden. They have been in contact with authorities such as the Swedish Medical Products Agency, the National Board of Health and Welfare and the Health and Social Care Inspectorate (IVO) regarding the issue of whether it is permissible to systematically treat patients with a drug that is not approved for these patients, and they have also contacted the Ministry of Health and Social Affairs to ask them to investigate the rules that apply to the free right of prescription. The authorities have announced that they do not see any problems and no response from the Ministry has been forthcoming.
The question of using rituximab against MS is of fundamental importance for the entire pharmaceutical sector, and not just in Sweden. The system of free prescription right is established in many countries across the world, and the USA is very interested in developments in Sweden, explains Fredrik Piehl. This interest has resulted in him and his research colleagues recently receiving eight million US dollars from an American national research institute to conduct a new study called SWEEP-MS to compare how things are going for Swedish MS patients in real life, a study that encompasses a longer period than that normally covered in standard clinical studies.
“We are starting now and we will include registry data from 2011 combined with a follow-up over five years, which means that, over a five-year period, we can gradually provide increasingly better outcome data,” he says.
A very large geographical difference
One feature of the somewhat unclear situation surrounding rituximab is that there is currently a very large geographical difference in Sweden in how it is used.
“You can interpret the evidence situation in different ways. There are those who say that rituximab is better than all other preparations and should be used for all MS patients. Then there are those who say that rituximab is not approved for MS and therefore should not be used at all. You could say that both views in any way are right,” says Fredrik Piehl.
The consequence has been that nine out of ten MS patients in Umeå are given rituximab, four out of ten in Stockholm, and only one of of ten are prescribed it in Skåne. Normally it is not preferable with large geographical differences in treatment, but for the SWEEP-MS study, this means that it will be possible to compare the results of different strategies in large patient groups.
“This study will address several key issues, not least the importance of administering highly effective treatment at an early stage to younger patients,” he says.
In other words, the future looks quite bright for MS patients. The researchers understand much more about the causes of the disease, there are plenty of new medicines and the doctors are beginning to learn how to use them. There is a new understanding of the disease process which at best will lead to highly effective treatment being administered early on and stopping inflammatory neuronal death, so that the patients can maybe avoid losing their nerve cells and thus never have to enter into the progressive phase.
That at least is the plan according to the researchers at Karolinska Institutet. Time will tell how successful the journey will be.
Facts about MS
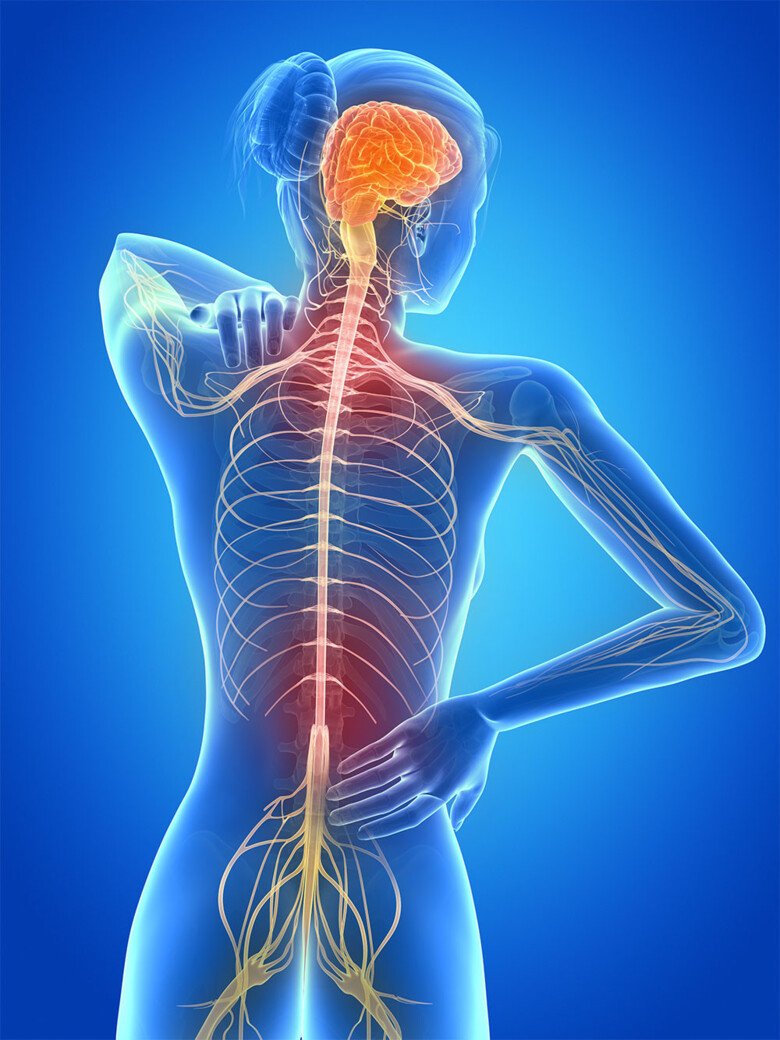
The prevailing hypothesis is that multiple sclerosis, MS, is an autoimmune disease where the body's immune system attacks the nerve fibres in the brain and spinal cord and destroys their “protective shield” of myelin. The symptoms depend on where in the brain and spinal cord neuronal death occurs. MS often manifests between the age of 20 and 40.
Usual initial symptom: Impaired vision in one eye due to optic neuritis. Numbness or altered sensation in the arm or leg.
Other symptoms: Reduced muscle strength, dizziness and coordination issues, walking problems.
The protective myelin around nerve fibres is attacked and destroyed by the body's own defence cells.
Two phases of the disease: Manifests often in a flare-up
During the first 15-20 years, the inflammatory activity is high and the nerves are attacked and destroyed. The inflammation then reduces while more and more symptoms appear, caused by a combination of the destroyed nerves and natural ageing.
- The majority of the patients, 80-90 per cent, initially experience a relapsing form of the illness, which means alternating periods of having symptoms and being asymptomatic.
- This relapsing form often transitions after 15-20 years to the second form which is called secondary-progressive MS, which means an increasing loss of physical functions with age.
- There is a third form called primary-progressive MS which is similar to secondary-progressive MS except that patients do not present with the relapsing form beforehand. It is likely that the disease has progressed but without showing symptoms.
Identified scars in the brain
The symptoms suffered by MS patients were first described nearly 200 years ago, and 150 years ago a French neurologist found during autopsies that the patients had hard scars in the brain and spinal cord, an aspect which gave rise to his naming of the condition multiple sclerosis, which means “many scars”.
The disease was described for the first time in a Swedish medical textbook exactly 100 years ago, and aside from rest, baths and massages, the recommendations included X-rays, arsenic and mercury ointment.
MS is increasing – among women
New cases of MS are slowly increasing in number in most parts of the world, as well as in Sweden. But the increase seems to be prevalent exclusively among women. In the early 1900s, the gender distribution of the disease was even, and an equal number of men and women were affected. In most older textbooks it says that the ratio is 2: 1, meaning twice as common among women as among men. But the latest research findings instead indicate the ratio to be 3:1.
No one knows why the disease is increasing among women. It is hypothesised that the increase in smoking among women is the cause, but in that case the incidence should instead decrease in a country like Sweden, where the proportion of smokers has decreased over time.
Text by Fredrik Hedlund, in translation from Swedish.
First published in Swedish in the magazine Medicinsk Vetenskap no 4, 2016.
