Lightning-fast vaccine development
The very first vaccines against the new corona virus are a breakthrough on several levels. Not only were they developed extremely fast, they are based on new technology whereby the vaccin is completed inside our bodies. But is the fastest technology also the one that protects us best?

Text: Ola Danielsson, first published in January 2021
Curious about the mRNA vaccine. There was no guarantee that there would be a vaccine at all. Just barely a year after the virus sars-cov2 appeared, several vaccines are approved and even more are on the way.
“It has exceeded all expectations,” says Matti Sällberg, professor of biomedical analysis at the Department of Laboratory Medicine, Karolinska Institutet.
Vaccines have saved millions of lives and are among the greatest successes within medicine. But it usually takes longer to develop a vaccine: the vaccine against measles, for example, took 28 years to develop. The vaccine against HPV which causes cancer, took 15 years. It took just as many years to develop the vaccine against rotavirus disease which causes diarrhoea. For some viruses, such as HIV, there is still no effective vaccine, despite decades of research.
But in 2020, vaccine development suddenly accelerated at rocket speed. Financial resources and diligent researchers are part of the explanation. But it is also due to the fact that the history of vaccines against corona virus actually began much earlier on.
“We didn't start from scratch when the new corona virus surfaced. We have been researching the SARS virus for 17 years and had already described the spike protein for example, that the virus uses to infect our cells,” says Matti Sällberg.
Mild cold symptoms
There are currently seven corona viruses that infect people, four of which cause mild cold symptoms. Awareness of the first harmless corona viruses developed in the 1960s and the first deadly corona virus, sars-cov, occurred in China in 2002. The second, mers-cov, was discovered in 2012 in Saudi Arabia.
Researchers began the development of a vaccine against both sars-cov and mers-cov. The strategy that seemed most promising was based on using genetic engineering to recreate a part of the virus's spike protein, the protruding part of the virus's surface that it uses to enter cells. The idea was that the vaccine would stimulate neutralizing antibodies that can block the virus from attaching to receptors in the cells.
The work was never completed before the epidemics subsided, but when sars-cov-2 appeared, the vision of a future vaccine was clear to the researchers. In addition, a new technology for rapid vaccine development was in the starting blocks – the mRNA vaccine.
But nor were these invented during the corona year 2020.

Karin Loré, professor of vaccine immunology at the Department of Medicine, Solna, Karolinska Institutet, explains that they are a long-awaited addition to humanity's vaccine arsenal.
“A vaccine is something that looks like a virus or other infectious agent and which can be used to create a memory in the immune system. When the real virus is exposed to the immune system, trained soldiers are already there waiting,” she says.
A classic way, historically, of developing a vaccine is to weaken a micro-organism, such as a virus, so that it no longer makes us sick. If the virus still stimulates our immune system, it could function as a vaccine.
“These live vaccines are often the best vaccines, because they look and behave mostly like the real disease-causing micro-organism,” says Karin Loré.
Live viruses
But live viruses can sometimes be too risky to use. Many vaccines therefore use killed viruses or only a small part of them, usually a protein that sits on the surface and is exposed to the immune system – just like the corona virus spike protein.
“A protein does not activate the immune system so strongly. Therefore, it may have to be administered on several occasions and combined with an adjuvant, a substance that excites the immune system a little extra,” says Karin Loré.
“Even though significant progress has been made with regard to the production techniques for protein, it can be a challenge to mass-produce proteins that have the correct appearance which must then be characterized and combined with the right adjuvant in order to become a working vaccine,” Karin Loré explains.
Scientists have always looked at how our own cells produce proteins: In the nucleus there is a blueprint for the body's proteins which is stored in the form of DNA sequences. If necessary, DNA is translated into messenger RNA (mRNA) which leaves the nucleus and provides instructions for the formation of protein.
The idea behind the mRNA vaccine is to smuggle the blueprint for viral protein into our cells in the form of mRNA molecules. The cells can then temporarily produce the viral protein, which in turn will develop an immune response.
As early as 1994, researchers at Karolinska Institutet showed that RNA can activate the immune system in mice. Since then, the technology has been refined in the vaccine field and in recent years scientists have tested mRNA vaccines against viruses such as influenza, rabies, Zika and Ebola in animals and humans.
Medical applications
Some companies such as BioNTech, Moderna and CureVac had been investing for several years in the medical applications of mRNA technology and they were well prepared when the corona pandemic threw the vaccine issue into the spotlight. Suddenly there was extreme urgency and the take-off ramp for the initiation of the development of an mRNA vaccine was short.
“You only need the genetic sequence, and it is basically enough to key it into the synthesis machine and you have laid the foundation for the new vaccine – it's fast,” says Karin Loré.
The genetic sequence for sars-cov-2 was published in mid-January 2020. Two months later, on 15 March 2020, Moderna had developed a vaccine candidate at record speed and started testing it on humans in clinical trials.
One advance in the research that made the vaccine possible is that scientists have learned to chemically modify the short-lived mRNA molecules to make them a little more stable. By packing mRNA into nanodrops of fat molecules, known as lipid nanoparticles, researchers have also developed a way to safely and efficiently deliver the mRNA vaccine into the cells.
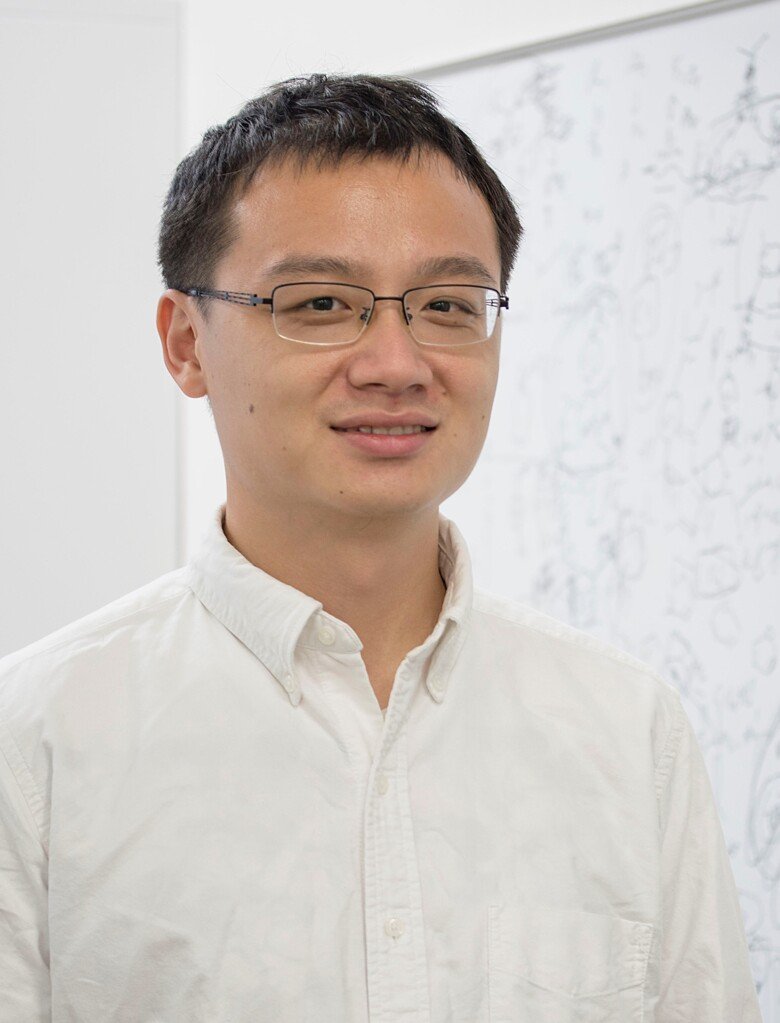
“mRNA is a large molecule that cannot enter the cell on its own. The lipid nanoparticles help the mRNA molecule to be absorbed by cells and escape degradation. In addition, they help activate the immune system,” says Linxian Li, research associate at Karolinska Institutet's Hong Kong branch, Ming Wai Lau Centre for Reparative Medicine, who has been working for ten years on the development of a delivery system for mRNA molecules.
Together with his former supervisor Robert Langer, American researcher and innovator and co-founder of Moderna, Linxian Li published a study in 2019 on how different types of lipid nanoparticles can be effectively produced and selected. Linxian Li hopes that his platform for the production of lipid nanoparticles will be used in several types of vaccines but also other types of mRNA therapies.
“The platform can be used to screen out better lipid nanoparticles with less side effects and a longer storage time. It can also be used to extend the use of mRNA from vaccine to gene therapy,” says Linxian Li.
Facts: Three vaccine records
The world's most productive vaccine creator was the American microbiologist Maurice Hilleman. He lived from 1919 to 2005, developing 40 vaccines that are believed to have saved millions of lives.
The world's first vaccine was developed in 1796 when the English physician Edward Jenner developed a vaccine against smallpox.
The world's only disease that was eradicated using a vaccine is smallpox.
Sources: Karin Loré, Wikipedia
With a known genetic sequence for the spike protein, stable mRNA molecules and functionalized lipid nanoparticles, it became possible to quickly take the mRNA technology all the way to an approved vaccine against covid-19.
But it was also based on the fact that the mechanisms for how mRNA vaccines work in the body had already been studied for some time. Karin Loré has been collaborating for several years with two of the companies that have invested in the technology, Curevac and Moderna.
”We have evaluated several of their vaccine candidates in trials with monkeys. We have tested them as vaccines against viruses such as rabies, influenza and even corona virus and tried to answer questions about how strong and what kind of immune response they induce and how long the vaccine remains in the body,” says Karin Loré.
A myth in social media
In social media groups, a myth has spread that the mRNA vaccine can combine with our genes.
“That's not true, mRNA cannot combine with our DNA and, in addition, the mRNA molecules are rapidly degraded. Most of the protein is produced in the first few days, but some protein remains after 10 days,” says Karin Loré.
The immune system reacts to the mRNA vaccine in two stages: First, there is a rapid reaction to the mRNA molecules themselves and the lipid nanoparticle. Then there is a slower specific response when the immune system builds up a memory against the virus protein.
“mRNA shouldn’t float around in the body, it's normally a sign of infection so the immune system reacts to it in a powerful way,” says Karin Loré.
During the rapid immune reaction, a molecule called type 1 interferon, among others, is produced, which in turn activates a number of immune cells. The process is part of the body's natural defence against a virus. The rapid immune response contributes to the vaccine's efficacy but can also lead to palpable side effects such as fever, redness and headaches.
A large number of studies will now follow up on the effects in the population of the vaccines against covid-19. According to Karin Loré, an important research issue is what the immune response will be and how the side effects differ between different groups of people.
“For example, it is not known whether mRNA vaccines are suitable for young children because such studies have not yet been carried out. However, it seems that it works well with older people, which is not the case for all types of vaccines. This may be because this rapid immune reaction contributes to a better specific response,” says Karin Loré.
All vaccines activate the immune system. It is never completely without risk, and at the same time, it is the reason why the vaccine works.
“Generally speaking, the risks are relatively minor compared to not getting vaccinated and having instead, to acquire a natural infection. But there may be groups that react more strongly than others and may prefer to take another covid-19 vaccine than those based on mRNA, it is important to continue to study this carefully,” Karin Loré explains.
Pharmaceutical companies
One concern is that the pharmaceutical companies have rushed the mRNA vaccines and that safety has been neglected. Karin Loré does not share this concern.
“There is still a lot to learn about mRNA vaccines, but safety has not actually been compromised when the vaccines were approved. The vaccines have been tested in large studies and the side effects, at least the most common, have already come to light. It is possible that more side effects will manifest themselves when even more studies have been carried out. But in that case they would be very rare,” says Karin Loré.
In the clinical trials conducted so far, the new mRNA vaccines have demonstrated good efficacy and safety. But Karin Loré does not believe that they are necessarily better than all other vaccines. Approximately 200 vaccines including most of the already established vaccine types are being developed to fight covid-19.
“For example, a protein vaccine will most likely work very well, it remains to be seen which vaccine will be the most efficacious against the corona virus,” says Karin Loré, who herself will take the vaccine she is offered, regardless of the type of vaccine it is.

Nor does Matti Sällberg expect the mRNA vaccine to be the only winner in the vaccine race. He believes that we will need a mix of vaccines that are used for different purposes and suit different groups.
One disadvantage of the mRNA vaccines approved so far is that they are sensitive to heat and need to be stored in a freezer. According to Matti Sällberg, they can also be difficult to produce in sufficient quantities.
“The biggest bottleneck is the lack of production facilities. Production facilities using this new technology are not in place around the world,” he says.
Developing a DNA vaccine
He himself is working on developing a DNA vaccine that targets more parts of the virus, not just the spike protein.
“We are slow compared to the big companies, but we believe that we can complement this rapid development by offering a vaccine that works against several corona variants,” says Matti Sällberg.
The DNA vaccine works in a similar way to the mRNA vaccine. The difference is that the genetic sequence that makes up the vaccine is a DNA molecule instead of an mRNA molecule.
“The advantage is that the vaccine can be stored at room temperature because DNA is a more stable molecule. It may also be an advantage that the vaccine is active a little longer in the body before it breaks down,” says Matti Sällberg.
The mRNA vaccines do their job in the cytoplasm in the cell, but DNA vaccines need help to get through another barrier, into the nucleus. At present, an electric pistol is used to provide a small electric shock that opens up pores in the nucleus.
“It's a disadvantage but not an insurmountable problem. This equipment is available in many hospitals, so DNA vaccines could already be used without problems by healthcare professionals, for example,” declares Matti Sällberg.
A clear advantage of both mRNA and DNA vaccines is their flexibility.
“If the virus's genetic code changes so that the vaccine no longer works, we can quickly update the vaccine accordingly. It could take perhaps two weeks,” states Matti Sällberg.
Provides lifelong immunity
It is not certain that vaccines can stop a disease that has been widely disseminated. A crucial factor is how long a vaccine provides immunity. It may be difficult to develop a vaccine that provides better immunity than natural infection.
“Measles, for example, provides lifelong immunity, and so too does the vaccine, for the most part. Common colds do not provide very long immunity, so neither would a vaccine probably. Common circulating seasonal corona viruses seem to be able to provide immunity that lasts one or two years and with sars-cov-2, we don't yet know,” says Karin Loré.
The research so far suggests that vaccination provides immunity for at least six months. Matti Sällberg believes that it may be enough to bring the pandemic under control and avoid recurring waves that overload the health care system, but that remains to be seen.
“It won’t work if all of humanity has to get vaccinated every three months, but once a year or less often, and we may be able to cope. We'll have to wait and see, but the way I see it, vaccines are the only way out,” says Matti Sällberg.
The dream is a universal corona vaccine that works against many virus variants and provides long immunity.
“It will be difficult, but it may be possible, which is why we need to continue the research.”
Text: Ola Danielsson, the article is produced for the magazine Medicinsk Vetenskap No. 1/2021.
First published in Swedish on ki.se in January 2021.
 Foto: Public Domain
Foto: Public DomainNew to the vaccine gang
The new mRNA vaccines are super smart inventions but so are old vaccines. Several different vaccine types are important in the fight against diseases such as covid-19.
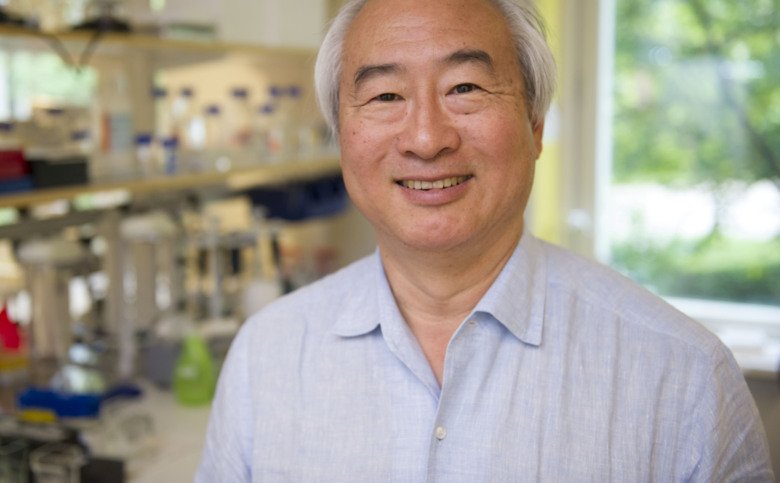 Foto: Ulf Sirborn
Foto: Ulf SirbornThe story about Moderna and the mRNA vaccine
The success of the mRNA-based vaccines is a boost for the entire mRNA field and can lead to new treatments for completely different diseases. This is the view of KI Professor Kenneth Chien, co-founder of Moderna, one of the companies that has developed a COVID-19 vaccine.
