The BONEMORE study
A clinical trial where we compare the effects of two training methods on bone strength and other important outcome measures for health. The study was carried out in 2021 to 2023.

The purpose of this study
- To investigate the effect of isometric axial loading (IAL), OsteoStrong, compared to dynamic multicomponent exercise (DME) on bone strength in older women with low bone mass
- For the primary outcome (Bone material strength index, BMSi) in the RCT 1, the aim is to investigate if the IAL is non-inferior (not worse than) to the DME
- To explore the participant's experiences and perceptions of the training methods
Why is this study important?
Osteoporosis and fragility fractures are a major public health problem worldwide. Fragility fractures result in major functional impairments and suffering, while worldwide medical care costs skyrocket every year. Osteoporosis is very common in the older population (women and men) and particularly in women.
Physical exercise is a very important part in prevention and treatment of osteoporosis and fragility fractures. Previous studies has found that physical exercise can reduce bone loss and prevent falls. However, the research on the effectiveness of exercise on bone quality, and bone markers that reflect bone remodulation, is very scarce. We also don't know whether isometric training can have positive effects on bone strength and other health-related factors. This study will increase the knowledge about these areas.
Study designs
- Randomized controlled trial
- Qualitative interview study
- Longitudinal study
Study population
A total of 194 women were included in the study. In the table below you can see the women’s baseline characteristics.
Table 1. Baseline characteristics.
| Parameter | IAL (n=97) | DME (n=97) |
|---|---|---|
| Age (median years, IQR) | 70 (67-75) | 70 (67-75) |
| Weight (mean kg, SD) | 64 ± 9 | 64 ± 9 |
| Height (mean cm, SD) | 163 ± 6 | 162 ± 6 |
| BMI (mean, SD) | 24.2 ± 3.4 | 24.1 ± 3.4 |
| Bonespecific drugs (n, %) | 11 (11 %) | 12 (12 %) |
| Previous fracture (n, %) | 48 (49 %) | 51 (54 %) |
| FRAX score MOF% (median, IQR) | 12 (9.1-19) | 13 (8.75-17) |
| FRAX score hip fracture % (median, IQR) | 1.9 (1-4) | 1.9 (0.9-3.9) |
| BMSi (mean, SD) | 73.87 ± 9.58 | 74.7 ± 9.73 |
| BMD LS Total (mean g/cm2, SD) | 0.873 ± 0.130 | 0.866 ± 0.129 |
| BMD FN Right (mean, SD) | 0.756 ± 0.101 | 0.763 ± 0.094 |
| BMD FN Left (mean, SD) | 0.753 ± 0.091 | 0.758 ± 0.084 |
| T-score LS Total (mean, SD) | -1.55 ± 1.24 | -1.68 ± 1.15 |
| T-score FN Right (mean, SD) | -0.847 ± 0.845 | -0.790 ± 0.786 |
| T-score FN Left (mean, SD) | -0.870 ± 0.762 | -0.830 ± 0.708 |
| P1NP (median, IQR) | 48.8 (37-63) | 47.6 (34-61) |
| Sclerostin (median, IQR) | 26.3 (20-32) | 25.8 (21-32) |
| BALP (median, IQR) | 20.1 (15-24) | 19.1 (15-23) |
| CTX (median, IQR) | 370 (257-503) | 370 (238-513) |
The inclusion criteria were:
- Women, 65-79 years of age
- T-score ≤-1.0 in the femoral neck or lumbar spine
- Vaccinated against Covid-19
- Ability to participate in the training for nine months
The exclusion criteria were:
- Ongoing treatment with bone-specific drugs with an onset within the last year or previous drug treatment that were terminated within the last five years
- Ongoing bone-specific drugs that had been delayed for more than eight months for denosumab and 18 months for bisphosphonates
- Ongoing treatment with oral corticosteroids (≥5 mg Prednisolone)
- Vertebral fractures that were diagnosed within the last three months, that had not been assessed by a physician, or had not been previously treated with bone-specific drugs
- Bilateral hip replacement
- Symptomatic disc herniation, inguinal herniation or umbilical herniation
- Untreated hypertension
- Other diseases that could affect the study results or participation (e.g., malignant diseases, secondary osteoporosis, muscle dystrophy)
- Conditions that would hinder the impact microindentation test (large edema, skin infection, allergy towards local anesthetics
- Ongoing or previous training at OsteoStrong™
Training methods
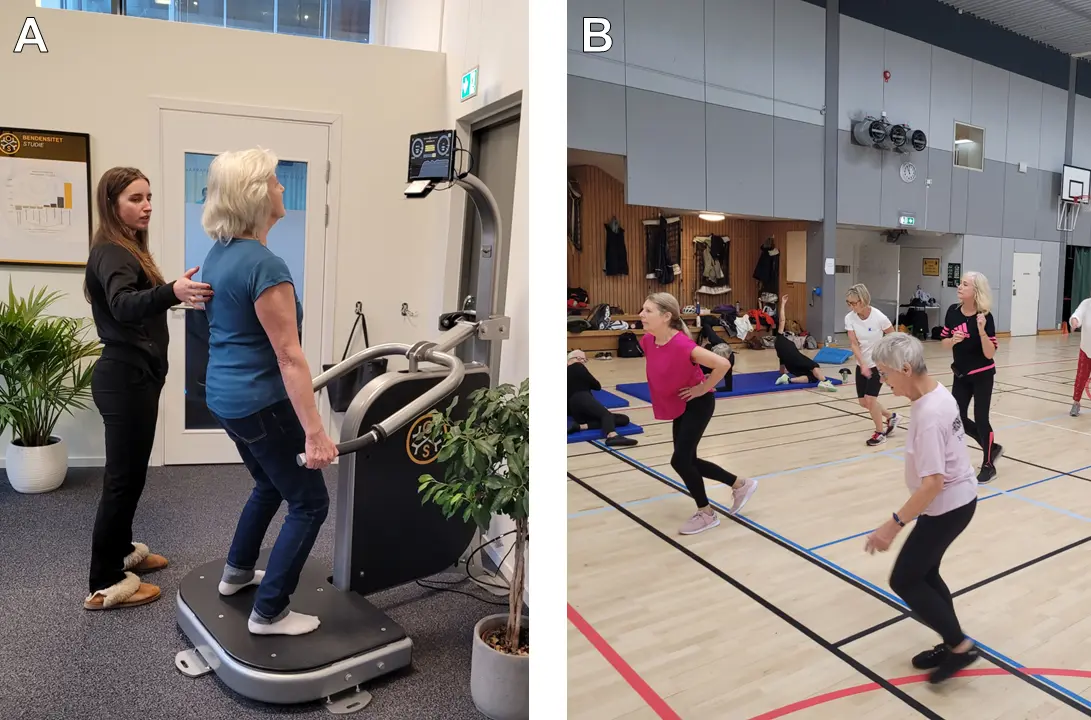
Training method A: Isometric axial loading (IAL) at OsteoStrong
The participants trained individually at the OsteoStrong studio in Solna, Sweden (one 20-minute session per week for nine months). Each session consisted of warm-up exercises on a vibration platform (including balance training), and isometric exercises (static loading) in four machines. The training was supervised by training instructors.
Specific Exercises:
- Balance on vibration platform (e.g. standing on one leg)
- Upper growth trigger (static chest press)
- Lower growth trigger (static leg press)
- Core growth trigger (static pull-down)
- Postural growth trigger (similar to a static deadlift)
Training method B: Dynamic multicompontent exercise (DME)
The participants train in a group, two 60-minute sessions per week, for nine months, at the Swedish School of Sport and Health Sciences (GIH). Each session consists of exercises based on current recommendations and previous research regarding exercise for osteoporosis. The sessions focus on strength, balance, coordination, mobility, and cardio fitness. The training was supervised by a training instructor.
Specific exercises in training session 1 (station-based training): warm-up, squats, supine hip thrusts, side-lying hip thrusts, side-to-side jumps, push-ups against the wall, light jumping while jogging, back extension in prone position, dead bug (core exercise), step-up, balance (e.g. standing on one leg, balance board).
Specific exercises in training session 2 (in the gym with machines): warm-up (treadmill, rowing, cross-trainer, bike), leg press, lats pull-down, row, back extension in belly-back, chest press, leg lift to the side (standing or lying down), balance (e.g. standing on one leg, balance board).
Measuring instruments and outcome measures
- Outcome measures for bone health: Bone material strength index (BMSi) via microindentation test, which is a measurement for the bone quality; bone mineral density (BMD) via Dual energy X-ray absorptiometry (DXA); bone markers via blood test, which reflects the bone remodeling process; vertebral fractures via vertebral fracture assessment (VFA).
- Questionnaires: Self-rated health (SF-36), Lifestyle habits, Falls efficacy scale (fear of falling), Downton fall risk index (fall risk), Osteoporosis questionnaire.
- Physical tests: Muscle strength, Muscle endurance, Balance tests, Balance with BTrackS™, Walking and movement tests
- Lung function: Dynamic spirometer (Welch Allyn).
- Physical behaviors: Accelerometer (detects body vibration or motion acceleration) and questionnaires, Physical activities and exercises documented daily in a diary that the participants maintain during the nine-month training period.
- Focus group interviews for the qualitative study.
Follow-ups
- All tests were conducted at baseline and after nine months of training, except for the bone markers, which were also measured at three months.
- Six months after the training had ended, surveys about physical activity, lifestyle, falls, and self-rated health, were sent out.
Preliminary results
In this study, a total of 194 women participated and were randomly assigned to either isometric axial loading (IAL) with OsteoStrong, or dynamic multicomponent exercise (DME) for nine months. The effect on the bone strength was measured through the participants' bone material strength index (BMSi; a measurement of the bone quality) using impact microindentation test on the shinbone, bone mineral density (BMD) via DXA-scan, and bone markers in the blood reflecting bone turnover. We also examined the occurrence of vertebral fractures before and after the training intervention.
Note that these are preliminary results, meaning that they have not yet been peer-reviewed and published, and might change. They must therefore be interpreted with caution.
Effects on bone strength
In summary, we saw no statistically significant differences between the training groups regarding BMSi, BMD, and bone markers at follow-up. However, we did observe improvements within the groups. In the OsteoStrong training, we saw a 2.9 percent increase in bone quality, and in the DME, we saw a 0.8 percent increase in BMD in the lumbar spine. We saw no changes in hip BMD. We also did not see any changes within or between the groups regarding bone markers.
Vertebral fractures
At the follow-up after nine months of training, we found four new cases of vertebral fractures(IAL: 3; DME: 1, chi2 p=0.312), two of which had occurred in accidents outside the study (one in each group). The remaining two (IAL: 2; DME: 0, chi2 p=0.155) cannot be conclusively linked to the training intervention.
Conclusion
Based on this study, the effect on BMSi (bone quality), BMD and bone markers did not differ between the OsteoStrong training and the dynamic multicomponent exercise. For the primary outcome (BMSi) in the RCT 1, the IAL was non-inferior (not worse than) to the DME.
Upcoming results
In addition to skeletal measurements, tests were conducted on muscle strength, muscle endurance, balance, walking speed, self-reported health, and lifestyle habits. We have also conducted a qualitative interview study. These analyses will be presented in upcoming articles and will provide further insights into the effects of the two training methods.
Links
Lead researcher
Helena Salminen
Senior Lecturer/Specialist PhysicianResearch team
Ann-Charlotte Grahn Kronhed, RPT, PhD, Associate Professor, Specialist in Geriatric health, Linköping University
Christina Kaijser Alin, RPT, PhD, Specialist in Geriatric health, Karolinska Institutet
Eva Andersson, PhD, Associate Professor, MD, Sports Physiologist, Swedish School of Sport and Health Sciences
Eva Toth-Pal, PhD, MD, Specialist in General Medicine, Karolinska Institutet
Hans Ranch Lundin, PhD, MD, Specialist in General Medicine, Karolinska Institutet
Kristin Møystad Michelet, PhD-candidate, MD, Karolinska Institutet
Maria Sääf, PhD, MD, Specialist in Endocrinology, Karolinska Institutet
Per Magnusson, Professor of Clinical Chemistry, Linköping University
Peter Lindberg, PhD-candidate, RPT, Specialist in Pain, Karolinska Institutet
Sven Nyrén, PhD, Associate Professor, MD, Specialist in Thoracic Radiology, Karolinska Institutet
Research principal
Region Stockholm
