Timeline: Contraceptives
For thousands of years, humans tried to separate sexuality and reproduction – for a long time not knowing how a child was conceived. Silkworms and sheep guts have both played their parts in creating the contraceptives that are available to us today.
Text: Mårten Göthlin, first published in Swedish in Medicinsk Vetenskap no 3/2017.
1800 BC Leaf-thin protection. It is likely the Egyptians were among the first to document their use of early forms of contraception. Ebers Papyrus rolls describe different diaphragms made from crocodile or elephant dung; fermented leaves and donkey milk were also used.

1839 Rubber used for first time. The very first condoms consisted of different types of cloth or animal guts and were developed as protection against venereal diseases thousands of years ago. The first rubber condoms were tailored in 1839, with mass production following 20 years later.
1876 Fusion. In Germany, researcher Oscar Hertwig observes an egg and sperm from two sea urchins fusing under a microscope for the first time. This discovery paves the way for research and hypotheses for use of contraceptives in the prevention of conception.

1930-1940 Hormone discoveries. Researchers from the USA and Germany discover and isolate human sex hormones (oestrogen, progesterone and testosterone) for the first time using several hundreds of litres of urine from pregnant women. These discoveries accelerate research into sex hormones for contraceptive purposes.
1957 A combination revolution. Contraception pioneer Margaret Sanger, her friend Katherine McCormick, researcher Gregory Pincus and gynaecologist John Rock develop the first contraceptive pill, a combination of synthetic progesterone and oestrogen. This gave women the option to take control of reproduction; use of the pill became widespread very quickly.
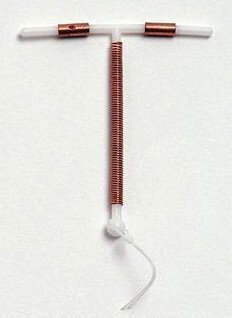
1960-70s Copper coils. Research Jaime A. Zipper discovers that implanting a small copper wire in the womb of rabbits stops them getting pregnant. A T-shaped plastic spiral with a copper wire provides new and effective protection against pregnancy; among other things, the copper hinders the sperms’ ability to move around.
According to the UN, use of contraceptives has increased by 80 percent since the 1970s. It is estimated that 18 billion condoms were used in 2015. At the same time, 225 million women still do not have any effective form of contraceptive that they can control themselves.
1966 Emergency protection. By circa 1920, researchers had already worked out that high doses of oestrogen could prevent pregnancy. Vets started to prescribe this hormone to animal owners whose dogs and horses were mating uncontrollably. The first emergency contraceptive pill for women, containing high levels of oestrogen, appeared in the 1960s.
1976 Positive spiral. Researcher Antonio Scommegna discovers that the progesterone in the womb causes changes to the mucous membrane, which is why bleeding reduces and also why conception is prevented. Later, the first hormone spiral is also developed, which releases synthetic progesterone (gestagen) locally in the womb.
1983 Implants. Researchers discover that silicone can be implanted in the body without rejection. The first rod implant consists of silicone mixed with gestagen, which is slowly released into the bloodstream. There are smaller variants, which are placed under the skin, available today.
![Photo: Jason Howle [cc-by]](/sites/kise/files/styles/article_full_width/public/qbank/apps_photo_jason_howle-custom20200807123332.jpg?itok=5YXLl6_h)
2016 Digital protection. The first contraceptive app, which indicates fertility using an accompanying thermometer, appears on the market. Karolinska Institutet tests apps aimed, among other things, at increasing young people’s use of condoms.
Sources: Thiery, European Journal of Obstetrics & Gynecology and Reproductive Biology 2000, Scientific Group on the Mechanism of Action, and Efficacy of Intrauterine Devices, WHO 1987, Ladipo & Akinso, African journal of reproductive health 2005, Pincus, Gregory, et al., American journal of obstetrics and gynecology 1958, Ellertson, Charlotte, International Family Planning Perspectives 1996, Cecilia Berger, UN Economic & Social Affairs, Trends in Contraceptive Use Worldwide 2015.
Contraceptives crucial for public health
People generally remain afraid of hormonal contraception, according to Cecilia Berger, a gynaecologist and researcher at the Department of Women's and Children's Health at Karolinska Institutet, who recently defended her doctoral thesis on the subject.

“This applies globally, but also in Sweden,” she says.
There are plenty of myths and misunderstandings surrounding the emergency contraceptive pill, and it’s not unheard of for it be confused with medical abortion, even among medical professionals.
One of the studies that feature in Cecilia Berger’s thesis provides evidence that ulipristal acetate, from the latest generation of emergency contraceptive pills, does not affect a fertilised egg’s ability to attach to the womb. We know from previous research, however, that it does delay ovulation. As such, it can be dismissed as some kind of abortion preparation.
“It’s important because it can increase acceptance of the emergency contraceptive pill among those who are in favour of the pill but against preparations that take effect after fertilisation has taken place. Emergency contraceptives are needed, for example, if use of other contraceptives has not gone to plan, or following a rape,” she says.
Having a global perspective is important to her:
“In low-income countries and areas affected by unrest and war without access to safe abortions, unwanted pregnancies are a direct threat to health. If women are able to choose if and when they fall pregnant, they have a completely different type of say in their health and socioeconomic status, and their future child’s health. The difference that contraceptives make to public health cannot be stressed enough,” Cecilia Berger tells us.
Future challenges
Contraceptives for men. Despite all that is known about male fertility, there is currently a lack of hormonal preparations for men. When it comes to developing these, gaining funding for clinical trials remains a major challenge. One study is currently underway in this area at Karolinska Institutet, however.
Finding alternatives without hormones. For medical reasons, many women cannot use oestrogen as a contraceptive, and some suffer from the side effects of synthetic progesterone (gestagen) as well. For these women in particular, it will be very important to develop non-hormonal methods.
Reaching out with information. Understanding why many who need protection still fail to use contraception is an important question that needs answering if we are to improve health, and in particular women’s health, around the world.
