COVID-19 BIC study to prevent suicide
The COVID-19 Brief Educational Motivational Awareness Increasing Intervention and Long-term follow-up program to prevent suicide (COVID-19 BIC): a clinical and epidemiological study
Background
The COVID-19 Brief Educational Motivational Awareness Increasing Intervention and Long-term follow-up program (COVID-19 BIC) is a study that has been developed by the National Centre for Suicide Research and Prevention of Mental Ill-Health (NASP) at Karolinska Institutet in collaboration with the World Health Organization (WHO). The COVID-19 BIC is adopted from the SUPRE-MISS study, a WHO multisite intervention that was conducted in early 2000s with the aim to reduce mortality associated with completed suicide. SUPRE-MISS was conducted in five countries namely Brazil, India, Sri Lanka, Islamic Republic of Iran and China. The effectiveness of SUPRE-MISS was evaluated and shown to have significant effect in reducing suicide rates in the treatment group that received the BIC in addition to treatment as usual in comparison with the control group which only received treatment as usual (1).
COVID-19 BIC will fit the context of the COVID-19 pandemic as well the cultural context of the different centers (2). The COVID-19 pandemic has become a life-changing crisis that has shaken everyone around the globe. Overnight, people have been put in isolation, in quarantine and many had to face the grim reality of unemployment, financial distress as well as the uncertain future for themselves and their families. The absence of protective factors such as connectedness and easy access to somatic and mental health care and the presence of risk factors such as isolation and unexpected threatening life events anticipate an increase in suicide rates.
The overall aim of the COVID-19 BIC study is to evaluate a treatment and prevention practice that aims at reducing morbidity and mortality associated with attempted and completed suicide, and to raise awareness about suicide, suicidal behaviors and mental health in different cultural and social backgrounds.
The study will be a multicenter randomized (1:1) control trial (RCT). Enrolment including eligibility screening and randomization into either the intervention or control group will be conducted according to the WHO randomization methods. Suicide attempters assigned to the COVID-19 BIC group will receive in-person motivational and awareness increasing interview using the COVID-19 BIC method (Annex 1) described separately. These interviews will be conducted by trained health care professionals (a doctor, a nurse, a psychiatrist, a psychologist) one day before or on the day of discharge. The patients in the BIC intervention group will be followed-up at 1,2,4, 8, 12 weeks and at 4,6,12,18 months by trained volunteers. The training for the health care professionals and volunteers will be given on a social medial platform where a group training will take place.
The COVID-19 BIC study will be carried out in the following WHO regions and countries and is implemented with the WHO office in Geneva.
| Africa | Americas | Europe | Asia |
|---|---|---|---|
| Ethiopia | USA | Italy | China |
| South Africa | Mexico | Romania | India |
| Kenya | Brazil | Spain | Kazakhstan (Eurasia) |
| Nigeria | Uruguay | Russia | Vietnam |
More countries can be included. Contact person Prof. Danuta Wasserman, Danuta.wasserman@ki.se
Methodology
The COVID-19 BIC study will be carried out in three sub-projects:
1. Epidemiological study
This study will be at a national level where aggregate data on each of the country’s situation during COVID-19 is analysed to study the difference among different countries. These data will include but not limited to number of affected individuals by COVID-19, number of deaths due to COVID-19, number of deaths due to suicide in relation to monetary investment for the pandemic, travel limitations, and lock down policies.
Additional data that can be retrieved from national registries in relation to COVID-19 will be added to the analyses.
This part will be designed and conducted by a group of social scientists, anthropologists and epidemiologists in collaboration with NASP.
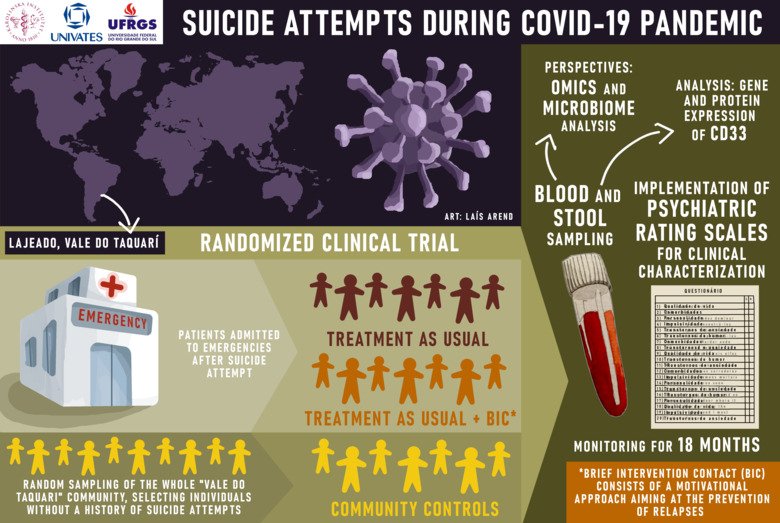
2. Clinical RCT study (COVID-19 BIC RCT): intervention study of suicide attempters who seek medical help
The study will be a multicenter randomized (1:1) control trial (RCT). Enrolment including eligibility screening and randomization into either the intervention or control group will be conducted according to the WHO randomization methods. Suicide attempters assigned to the COVID-19 BIC group will receive in-person motivational and awareness increasing interview on top of treatment as usual (TAU). These interviews will be conducted by trained health care professionals (eg: a doctor, a nurse, a psychiatrist, a psychologist) one day before or on the day of discharge. The training for the health care professionals will be given on a social medial platform where a group training will take place. The COVID-19 BIC will include nine follow-ups post discharge (1,2,4, 8, 12 weeks and at 4,6,12 months) with a final 18-months follow-up. Suicide attempters in the TAU group will receive TAU per the standard guidelines at the respective emergency departments (eg: routine or systematic psychiatric and/or psychological assessment) and a follow-up at 18 months. As the main hypothesis for is that the COVID-19 BIC will significantly lead to a reduced death by suicide at 18-months follow-up than treatment as usual, the main outcome measure is death from suicide at 18-month follow-up.
3. Community survey: survey of the community
A random sample of study participants will be selected from the same source population from which the suicide attempters are recruited for the clinical RCT study. The sample can be either randomly selected from national registers, voting lists or housing registers. Study participants will be selected at random and surveyed via telephone or in-person interview using standardized questionnaire. This standardized questionnaire aims to identify suicidal behavior and suicidal thinking among people, who, for various, reasons, do no present at the emergency department as suicide attempters. The survey will include sociodemographic questionnaires, suicide attempt history and family data, physical health, contact with health services and mental health as well as COVID-19 related suicide questions and questions which address community stress and problems. (3).
Significance
The present study, COVID-19 BIC, is a timely study that was designed due to the COVID-19 pandemic that started in late 2019 (2). The pandemic has become a life-changing crisis that has shaken everyone around the globe. The current study has the potential to have a global impact in regard to mental health promotion and suicide treatment and prevention as the study involves more many countries and continents with different cultural and social background and will contribute to a global awareness of mental health. While the study will draw similarities of mental health problems and suicide prevention and treatment effectiveness across different countries, it will also pinpoint important differences among these countries.
References
1. Effectiveness of brief intervention and contact for suicide attempters: a randomized controlled trial in five countries.
Fleischmann A, Bertolote JM, Wasserman D, De Leo D, Bolhari J, Botega NJ, et al.
Bull. World Health Organ. 2008 Sep;86(9):703-9
2. Wasserman D, Iosue M, Wuestefeld A, Carli V. Adaptation of evidence-based suicide prevention strategies during and after COVID-19 pandemic. World Psychiatry 2020;19(3).
3. Bertolote, J., Fleischmann, A., De Leo, D., Bolhari, J., Botega, N., De Silva, D., . . . Wasserman, D. (2005). Suicide attempts, plans, and ideation in culturally diverse sites: The WHO SUPRE-MISS community survey. Psychological Medicine, 35(10), 1457-1465.
Contact
Sweden - Coordinating Centre
National Centre for Suicide Research and Prevention of Mental ill Health (NASP)
Danuta Wasserman
Professor of Psychiatry and Suicidology, Head of NASP, Principal Investigator for the COVID-19 BIC studyAmericas Region
Mexico

Dr. Bernando Ng
Clinical Assistant Professor, Mexican Psychiatry Association, Principal InvestigatorDr. Thelma Sanchez
Principal InvestigatorUSA

Dr. Natalie Riblet
Trainer in the delivery of the COVID-19 BIC intervention, White River Junction VA Medical Center, Geisel School of Medicine at DartmouthUruguay
Dr. Silvia Pelaez
Psychiatrist, Uruguayan Psychiatry Association, Principal InvestigatorDr. Rafael Sibils
Psychiatrist and Psychotherapist, Uruguayan Psychiatry Association, Principal InvestigatorBrazil
Dr. Flavio Shansis
Clinical Assistant Professor, Brazil Psychiatric Association, Principal InvestigatorAfrican Region
South Africa
Discipline of Psychiatry, School of Clinical Medicine, College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa, https://ukzn.ac.za

Dr. Saeeda Paruk
Child Psychiatrist & research coordinator, Principal Investigator
Professor Bonginkosi Chiliza
Professor of Psychiatry, Co-investigator
Dr. Vidette Juby
Specialist Psychiatrist & researcher, Co-investigatorEthiopia
Dr. Askalemariam Bikiss
Principal Investigator, St.Paul Hospital Millennium Medical CollegeDr. Mohammed Negussie
Principal Investigator, Amanuel Mental Specialized HospitalKenya
University of Nairobi, Africa Mental Health Research and Training Foundation

Professor David M.Ndetei
Professor of Psychiatry, Principal Investigator
