Research Areas - Global Surgery
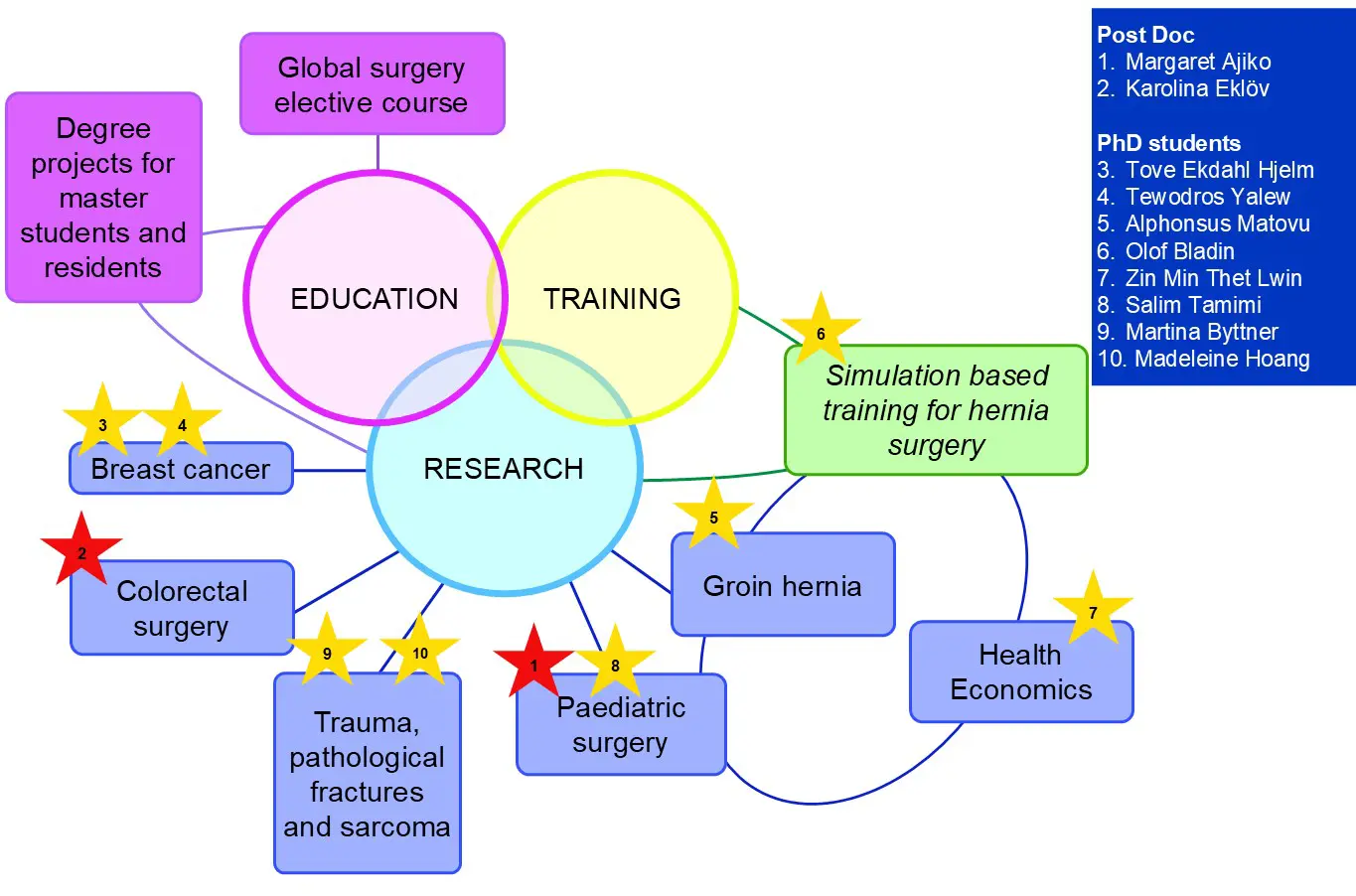
Research at Global Surgery Stockholm is predominantly clinical and involves surgery and allied specialities including oncology, clinical genetics and pathology. It is oriented towards clinical trials that assess innovative approaches to issues related to both quality and quantity of surgical services in low-resource settings.
Methods further include population-based epidemiological research, health-economic evaluation and qualitative research. Additional projects coupling low-resource settings with high-resource settings are part of the research agenda.
Our PhD students frequently have sub-studies both in Sweden and in low- or middle-income countries.
Groin Hernia
Throughout the world, 220 million people live with groin hernia (1), and groin hernia repair is the most common general surgical procedure worldwide. In high-income settings, the lifetime prevalence of groin hernia repair in men is 27% and in women 3% (2). The prevalence of groin hernia in men is around 10% (3)(4) and less in women. Hernia repair is the commonest general surgical procedure worldwide. Using mesh to achieve a tension-free inguinal hernia repair is the gold standard in hernia repair as it significantly reduces the risk of recurrence in men (5). Based on clinical trials by our team with partners in Uganda, Ghana and Sierra Leone, we can conclude that mesh hernia repair under local anaesthesia as day-case surgery for elective hernia repair in men is effective, safe and very cost-effective even in low-income settings. Clinical outcomes after mesh hernia repair in men performed by senior consultant surgeons, specialist surgeons, medical doctors with no formal surgical training and associate clinicians, are similar (6)(7) (8)(9).
Task sharing in groin hernia surgery is part of the solution for the high burden of unmet need for this procedure. However, task sharing alone cannot solve the human resource crisis: more surgical providers of all categories are needed. Finding out how best to train novices rapidly to perform safe and effective groin hernia repair is the next step in the research relating to groin hernia and task sharing. Olof Bladin, MD, will investigate surgical training, learning curves and the role of simulation-based learning for groin hernia repair.
In high-income settings, women account for less than 10% of adult groin hernia patients, but women have a higher risk of adverse outcomes, including death, than men (10). It is therefore recommended that groin hernia in women should always be repaired (11). In Uganda, women make up 18-24% of groin hernia repair patients (12)(13). In contrast to men, the evidence for open hernia repair in women is poor and more research is needed. Alphonsus Matovu, MD and general surgeon, is leading the projects on groin hernia and groin hernia surgery in women.
Health economical evaluation of the burden of hernia disease as well as the potential economical gains of scaling up surgery services is key in order to promote accessible surgery for all. Dr Zin Min Thet Lwin, MD and health economist, is leading the health economical project.
Project 1. Methods in mesh hernia repair in women – a double-blinded, randomised trial in Uganda
In a double-blinded, randomised trial, two methods of open-mesh hernia repair in women are compared. The first method is Lichtenstein's anterior groin hernia mesh repair. The second is a modified anterior mesh repair where the transversalis fascia is opened and the femoral region assessed for femoral hernia. A small slit of the mesh is thereafter sutured to the ligament of Cooper. The patients are adult women without significant comorbidities and with primary groin hernia. All the operations are conducted under local anaesthesia, as day-case surgery, by consultant surgeons.
The study was initiated in 2019 and 200 patients have been included and followed up after one year.
Project 2. Simulation-based learning in groin hernia repair
Together with partners at the Mayo Clinic, we have developed a 3D-printed hernia model with replaceable layers representing the abdominal wall. This model is be implemented in surgical training in a prospective cohort study in Sierra Leone and in a randomised trial in Uganda and Sweden. The hypothesis is that simulated training on a model will steepen the trainees' learning curve towards proficiency in hernia repair. This may save time and resources in places where the surgeons are too few to train the number of surgical providers needed. Trial registration (Sierra Leone)Trial registration (Sweden)
Project 3. Health economics and groin hernia repair
Health-economic evaluation of surgical programmes is essential to promote sufficient services and surgical training.
In this surgical project, the economic burden of groin hernia in sub-Saharan Africa will be investigated. The cost-effectiveness of providing open-mesh repair for all patients with
symptomatic groin hernias, through task sharing in this region, will be defined as will the willingness to pay for the operation in communities in Ghana, Sierra Leone and Uganda.
Primary patient outcome data from clinical trials on groin hernia repair in children, women and men in Uganda, Sierra Leone and Ghana will be used. Costs of the surgical procedures have been/will be collected along with these studies. Requirements for the surgical training will be obtained through key-informant interviews with lead specialist surgeons, and willingness to pay for the operation will be assessed through interviews with groin-hernia patients or their family members in these countries.
Discrete-event simulation will be performed, as will thematic analysis of the qualitative data. Stated-preference willingness to pay for the repair will be measured with contingent valuation. Multivariate regression of the estimated values will be tested against the respondents’ sociodemographic background.
Paediatric surgery
In low-income countries, children constitute a large proportion of the populations, and a considerable part of all surgical conditions affect children. A survey in Uganda, Sierra Leone, Rwanda and Nepal found that 19% of children (0-18 years) had a surgical need, unmet in 62% of cases (14). The estimated lifetime prevalence of surgical conditions in children in Uganda is 14.0 % (15). Many of these conditions could be treated successfully with surgery. Injuries and congenital anomalies account for a large proportion of paediatric surgical cases. Untreated, they contribute to lifelong disability and a considerable burden of disease. In addition, studies show high mortality rates after paediatric surgery.
Dr Mary Margaret Ajiko, is a general surgeon with a passion for children. Through her research, we have showed a prevalence of surgical conditions in children of 16% and a current unmet need for surgery of 6.3% (16). This means that over a million children need a surgical procedure, but there are only three paediatric surgeons in Uganda. Nationally in the public-health-care sector, surgery was performed mostly for congenital anomalies, inflammation and infection, and trauma. Of the procedures, 60% were performed by specialists in surgical disciplines, and anaesthesia was administered by physician anaesthesiologists in 12% of the cases (17). Obstacles to paediatric surgery relate to issues with infrastructure, and financial limitation. Power imbalances in societies where mothers are not authorised to make decisions to seek healthcare for their children are also part of the problem. Possible solutions include increasing awareness in the communities as well as the formation of regional referral hospital teams dedicated to surgery for children in (18).
Dr Salim Tamimi is a general surgeon and paediatric surgery fellow. He will build on the previous work relating to surgery for children in Uganda. A randomised trial on groin hernia surgery for children aged 1-12 years old will be carried out in Regional Referral Hospitals in Uganda and the safety of the task sharing between general surgeons and non specialist medical doctors will be assessed. Planning is in progress for this study and intended study start is mid 2024.
Breast cancer
With half a million deaths annually, breast cancer is a mass killer in women. In low-income countries such as Uganda and Ethiopia, young women present with advanced, incurable disease (19)(20). The five-year overall survival rate in breast cancer in Africa is half the 90% seen in Sweden (21)(22). Access to and utilisation of breast surgery in Uganda is extremely limited and only a small fraction of the estimated incidence of breast cancer receives surgical intervention (23).
Early-onset breast cancer in women and breast cancer in men have a high chance of being associated with mutations in certain genes such as the BRCA 1 and 2 genes. Genetic analysis is not routine in most low-resource countries and the prevalence of such mutations is unknown.
In this project, led by Dr Tove Ekdahl Hjelm and DrTewodros Yalew, women with early-onset breast cancer and men with breast cancer will be included. Tumour biology will be investigated and the existence of mutations in the BRCA 1 and 2 genes will be investigated, along with several additional genes. The patients will be followed for one year and adherence to recommended treatment will be investigated. Inclusion of patients in the study has been completed and analysis is in process. A qualitative study will investigate the acceptability of genetic investigation in this patient population and their first-degree relatives. A further study will investigate the usefulness and accuracy of artificial intelligence for histopathological diagnosis of breast cancer. Five hundred breast cancer tumour blocks will be used for this.
Identifying families at increased risk and target screening activities for them is a better option than population-wide screening for breast lesions in women in low- and middle-income countries, where financial resources are extremely limited. This research has potential to lead to cost-effective, risk- based screening and treatment as well as improved outcomes in the world’s poorest countries where most breast cancer mortality occurs.
Colorectal surgery
Colorectal disease in general, and colorectal cancer in particular, represent a considerable burden of disease worldwide. Due to epidemiologic transition, the burden of disease caused by colorectal illness is expected to increase in low- and middle-income countries. Very little research on surgical management of colorectal disease in such settings exists, and this vitiates the development of best practices and appropriate solutions. The studies will describe current practices in colorectal surgery and will relate them to outcomes in terms of complications and quality of life. This will fill important knowledge gaps, and the information can be used for policy-making and advocacy. The project will also form a platform for collaboration between the study partners through which future research can be planned and implemented. The project and this partnership can potentially improve the care of patients with colorectal cancer.
The project is led by Dr Karolina Eklöv together with partners at Tikur Anbessa Specialized Hospital in Addis Ababa, Ethiopia. Dr Eklöv is affiliated at the Department of Clinical Science and Education, at KI-SÖS.
Orthopaedics – injuries, infection and cancer
With 4.4 million deaths annually, injury is a leading cause of death for people in low and middle-income countries. Many millions more live with temporary or permanent disability following these injuries (24). Orthopaedic injuries are often non-fatal but if not appropriately managed, they can lead to lifelong disability. A combination of prevention efforts and improved surgical services are required to reduce lives and limbs lost due to trauma in LMIC.
Pathological fractures can occur as a result of osteomyelitis and bone metastasis. Bone metastases and associated pathological fractures often cause severe pain, loss of mobility and neurological deficits, leading to diminished quality of life of these patients. Surgical management is necessary when the long bones of the extremities are involved and is undertaken to reduce pain and improve function and quality of life of patients. Pathological fractures from osteomyelitis are preventable through infection prevention and control as well as adequate and timely management with antibiotics and sometimes surgery. Osteomyelitis is a common reason for surgery for children in Uganda (25). In depth analysis of the delays to treatment and the outcomes of surgical management of pathological fractures is essential as the case load of metastastic bone disease is expected to increase as the cancer incidence in LMICs is increasing.
Sarcoma represents a rare disease in the population but it accumulates in orthopaedic centres, in particular at Mulago National Referral Hospital. Patients often present late and outcomes are discouraging. There is a paucity of research on sarcoma and sarcoma surgery in Sub-Saharan Africa.
In this project, data on trauma, pathological fractures and sarcoma will be collected prospectively from the departments of orthopaedic surgery at the National Referral Hospital in Kampala, the Regional Referral Hospital in Jinja, both in Uganda. A qualitative study investigating barriers to care for pathological fractures will be carried out. PhD students Martina Byttnerand Madeleine Hoang will initiate the project together with Ugandan partners during 2025.
References
- DCP3 Hernia and Hydrocele [Internet]. [cited 2015 Apr 8]. Available from: http://www.dcp-3.org//chapter/1772/hernia-and-hydrocele
- Primatesta P, Goldacre MJ. Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol. 1996 Aug;25(4):835–9.
- Ohene-Yeboah M, Beard JH, Frimpong-Twumasi B, Koranteng A, Mensah S. Prevalence of Inguinal Hernia in Adult Men in the Ashanti Region of Ghana. World J Surg. 2016 Apr;40(4):806–12.
- Löfgren J, Makumbi F, Galiwango E, Nordin P, Ibingira C, Forsberg BC, et al. Prevalence of treated and untreated groin hernia in eastern Uganda. Br J Surg. 2014 May;101(6):728–34.
- Grant AM, EU Hernia Trialists Collaboration. Open mesh versus non-mesh repair of groin hernia: meta-analysis of randomised trials based on individual patient data [corrected]. Hernia. 2002 Sep;6(3):130–6.
- Beard JH, Ohene-Yeboah M, Tabiri S, Amoako JKA, Abantanga FA, Sims CA, et al. Outcomes After Inguinal Hernia Repair With Mesh Performed by Medical Doctors and Surgeons in Ghana. JAMA Surg. 2019 01;154(9):853–9.
- Löfgren J, Nordin P, Ibingira C, Matovu A, Galiwango E, Wladis A. A Randomized Trial of Low-Cost Mesh in Groin Hernia Repair. N Engl J Med. 2016 Jan 14;374(2):146–53.
- Löfgren J, Matovu A, Wladis A, Ibingira C, Nordin P, Galiwango E, et al. Cost-effectiveness of groin hernia repair from a randomized clinical trial comparing commercial versus low-cost mesh in a low-income country. Br J Surg. 2017 Feb 16;
- Ashley T, Ashley H, Wladis A, Bolkan HA, van Duinen AJ, Beard JH, et al. Outcomes After Elective Inguinal Hernia Repair Performed by Associate Clinicians vs Medical Doctors in Sierra Leone: A Randomized Clinical Trial. JAMA Netw Open. 2021 Jan 11;4(1):e2032681.
- Nilsson H, Nilsson E, Angerås U, Nordin P. Mortality after groin hernia surgery: delay of treatment and cause of death. Hernia. 2011 Jun;15(3):301–7.
- Miserez M, Peeters E, Aufenacker T, Bouillot JL, Campanelli G, Conze J, et al. Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2014 Apr;18(2):151–63.
- Matovu A, Nordin P, Wladis A, Ajiko MM, Löfgren J. Groin Hernia Surgery in Uganda: Caseloads and Practices at Hospitals Operating Within the Publicly Funded Healthcare Sector. World J Surg. 2020;44(10):3277–83.
- Löfgren J, Kadobera D, Forsberg BC, Mulowooza J, Wladis A, Nordin P. District-level surgery in Uganda: Indications, interventions and perioperative mortality. Surgery. 2015 May 6;
- Butler EK, Tran TM, Nagarajan N, Canner J, Fuller AT, Kushner A, et al. Epidemiology of pediatric surgical needs in low-income countries. PLoS ONE. 2017;12(3):e0170968.
- Butler EK, Tran TM, Fuller AT, Brammell A, Vissoci JR, de Andrade L, et al. Quantifying the pediatric surgical need in Uganda: results of a nationwide cross-sectional, household survey. Pediatr Surg Int. 2016;32(11):1075–85.
- Ajiko MM, Weidman V, Nordin P, Wladis A, Löfgren J. Prevalence of Paediatric Surgical Conditions in Eastern Uganda: A Cross-Sectional Study. World J Surg. 2022 Mar;46(3):701–8.
- Surgical procedures for children in the public healthcare sector: a nationwide, facility-based study in Uganda | BMJ Open [Internet]. [cited 2021 Sep 15]. Available from: https://bmjopen.bmj.com/content/11/7/e048540
- Ajiko MM, Löfgren J, Ekblad S. Barriers and potential solutions for improved surgical care for children with hernia in Eastern Uganda. Sci Rep. 2021 May 31;11(1):11344.
- Ersumo T. Breast Cancer in an Ethiopian Population, Addis Ababa. East and Central African Journal of Surgery. 2006 Jan 1;11(1):81–6.
- Kantelhardt EJ, Zerche P, Mathewos A, Trocchi P, Addissie A, Aynalem A, et al. Breast cancer survival in Ethiopia: a cohort study of 1,070 women. Int J Cancer. 2014 Aug 1;135(3):702–9.
- Styrgruppen för nationella bröstcancerregistret. Årsrapport, Rapport från nationella bröstcancerregistret 2014 [Internet]. [cited 2016 Jan 23]. Available from: http://www.cancercentrum.se/globalassets/cancerdiagnoser/brost/kvalitet…
- Sankaranarayanan R, Swaminathan R, Brenner H, Chen K, Chia KS, Chen JG, et al. Cancer survival in Africa, Asia, and Central America: a population-based study. Lancet Oncol. 2010 Feb;11(2):165–73.
- Hjelm TE, Matovu A, Mugisha N, Löfgren J. Breast cancer care in Uganda: A multicenter study on the frequency of breast cancer surgery in relation to the incidence of breast cancer. PLOS ONE. 2019 Jul 11;14(7):e0219601.
- Injuries and violence [Internet]. [cited 2022 Mar 6]. Available from: https://www.who.int/news-room/fact-sheets/detail/injuries-and-violence
- Ajiko MM, Kressner J, Matovu A, Nordin P, Wladis A, Löfgren J. Surgical procedures for children in the public healthcare sector: a nationwide, facility-based study in Uganda. BMJ Open.
