SPARKS – The health and social protection action research and knowledge sharing network
The Health and Social Protection Action Research & Knowledge Sharing network (SPARKS) is a global network created to facilitate action-oriented research on the public health impact of social protection, with a main focus on low- and middle-income countries.
SPARKS facilitates networking between prominent research institutions, public health practitioners, international organizations and civil society in order to catalyze and coordinate interdisciplinary action, research and knowledge sharing, develop a common priority research agenda, generate evidence and mobilize financial resources. SPARKS Network Members are located all over the world and come from 22 different countries and 27 organisations.
What we do
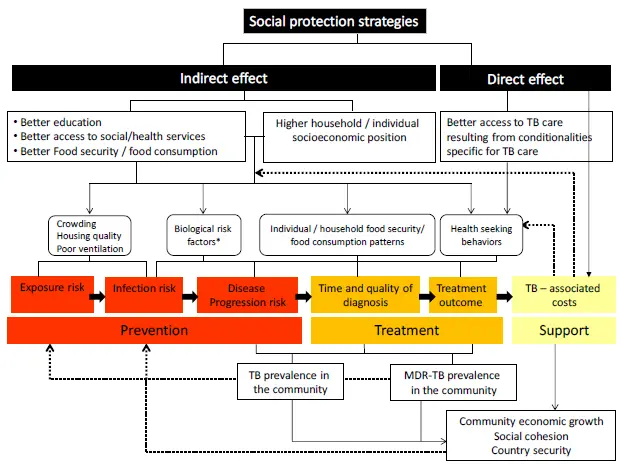
Our multi-sectoral team characterizes and evaluates the indirect and direct effects of social protection strategies on health, economic, and wider outcomes. With respect to TB, the archetypal disease of poverty, we aim to identify and address upstream and downstream social determinants at the individual, household, community, and governmental level, which influence risk of TB exposure, infection, disease, and cure.
Why we do it
The SDG Agenda offers a unique mandate and framework to advocate for a holistic approach to public health able to account for the multidimensional determinants of health and drivers of illness. There is a need to build upon the SDG framework and generate the necessary bulk of impact and operational evidence to turn this interdisciplinary vision into a truly interdisciplinary approach able to grant effective and sustainable solutions to major global health challenges.
Social protection is at the intersection of the development and health agenda. Nonetheless, the research into the public health potential of social protection schemes is still fragmented, especially in LMIC. For example, although cash transfer schemes are already an element of the response to health challenges in many countries, their impact on health-related outcomes has been only partially demonstrated and poorly understood: several large reviews concluded that conditional cash transfers have an impact on improving beneficiaries health behaviours, the magnitude of which seems to vary across countries and initiatives. The impact on health outcomes is less consistent, with evidence suggesting some effect on improving nutritional status, child growth and adult morbidity status, but not on maternal health, malaria and diarrhoea. These results are consistent with what is also known for HIV/AIDS: while there seems to be a positive impact on sexual behaviours, the impact on actual HIV outcome has been documented only in one study.
Not only is impact evidence limited and fragmented, but also the mechanism through which the impact of social protection strategies operate remains unclear. Achieving a sufficient level of understanding is crucial to design and implement public-health relevant social protection strategies, but also to understand why some interventions do not achieve the expected impact. Finally, it remains unknown how the scope of these schemes can be effectively and cost-effectively broadened to encompass public health objectives, while preserving their primary objective to protect people from poverty.
Given the broad scope and complexity of such agenda it is unlikely that one single research group will successfully fill the knowledge gaps. A network approach based on the share of knowledge and expertise as well as of existing platforms and opportunities may represent a far more efficient way to optimise financial and intellectual resources available. The SPARKS network was created with this rationale and with the aim of efficiently moving towards a more action-oriented type of research to ultimately tackle health inequalities.
Selected List of Publications from SPARKS Network Members:
- Social policy in Brazil (2004–2014): an overview – Social policy has played a central role in developing countries over the last decade, contributing to a significant decline in poverty and inequality. The objective of this paper is to provide an overview of the evolution of social policy in Brazil, its effects on inequality and poverty, and the implications of the current political and economic scenario regarding the maintenance of its continuous progress. (Patrícia Andrade de Oliveira e Silva, International Policy Centre for Inclusive Growth 2017)
- Catastrophic health costs averted by TB control: findings for India and South Africa from a modeling study: The economic burden on households affected by tuberculosis through costs to patients can be catastrophic. WHO’s End TB Strategy recognises and aims to eliminate these potentially devastating economic effects. We assessed whether aggressive expansion of tuberculosis services might reduce catastrophic costs. (Stéphane Verguet, The Lancet 2017)
- Comparison of two cash transfer strategies to prevent catastrophic costs for poor tuberculosis-affected households in low- and middle-income countries: An economic modelling study Social protection initiatives, including cash transfers, are endorsed to help prevent catastrophic costs. With this aim, cash transfers may either be provided to defray TB-related costs of households with a confirmed TB diagnosis; or to increase income of households with high TB risk to strengthen their economic resilience. We undertook an economic modelling study from the patient perspective to compare the potential of these 2 cash transfer approaches to prevent catastrophic costs. (William E. Rudgard, PLOS Medicine 2017)
- Modelling the social and structural determinants of TB: opportunities and challenges: Despite the close link between tuberculosis (TB) and poverty, most mathematical models of TB have not addressed underlying social and structural determinants. We reviewed studies employing mathematical modelling to evaluate the epidemiological impact of the structural determinants of TB. (Debora Pedrazzoli, The International Journal of Tuberculosis and Lung Diseases 2017)
- Uptake of governmental social protection and financial hardship amongst drug-resistant tuberculosis treatment in Rio de Janeiro, Brazil:In May 2016, there were 1601 people with drug-resistant TB in Brazil, with 29% residing in Rio de Janeiro state. To evaluate whether uptake of social protection during treatment is associated with reduced risk of experiencing financial hardship, a cross-sectional survey of people with drug-resistant TB who had been receiving treatment for at least 1 month and were attending an outpatient clinic in Rio de Janeiro state was conducted. The uptake of social protection was associated with lower risk of incurring total costs ≥20% of household income, impoverishment and experiencing all three hardships, but not with using a coping strategy. (William E. Rudgard, European Respiratory Journal 2018)
- Addressing social determinants to end tuberculosis: Leave no one behind. This is the overarching pledge of the Sustainable Development Goals; a pledge that is far from being realised. In 2016, more than 4 million people with tuberculosis were estimated to be undiagnosed or their care and treatment were unknown. In the same year, nearly a fifth of the people who were diagnosed and known to be treated for tuberculosis had adverse outcomes, including 1·3 million deaths. One reason that millions of people affected by tuberculosis are left behind is an absence of coordinated, international action to combat poverty and inequality. (Tom Wingfield, The Lancet 2018)
- The impact of social protection and poverty elimination on the End TB strategy targets: a statistical model of Sustainable Development Goal: The End TB Strategy and the Sustainable Development Goals (SDGs) are intimately linked by their common targets and approaches. SDG 1 aims to end extreme poverty and expand social protection coverage by 2030. Achievement of SDG 1 is likely to affect the tuberculosis epidemic through a range of pathways. We estimate the reduction in global tuberculosis incidence that could be obtained by reaching SDG 1. (Daniel Carter, The Lancet 2018)
- Modelling the impact of social protection on tuberculosis: the S-PROTECT project – Tackling the social determinants of Tuberculosis (TB) through social protection is a key element of the post-2015 End TB Strategy. However, evidence informing policies are still scarce. Mathematical modelling has the potential to contribute to fill this knowledge gap, but existing models are inadequate. The S-PROTECT consortium aimed to develop an innovative mathematical modelling approach to better understand the role of social protection to improve TB care, prevention and control. (Delia Boccia, BMC Public Health 2018)
- How affordable is TB care? Findings from a nationwide TB patient cost survey in Ghana – Tuberculosis (TB) is known as a disease of the poor. Despite TB diagnosis and care usually being offered for free, TB patients can still face substantial costs, especially in the context of multi-drug resistance (MDR). The End TB Strategy calls for zero TB-affected families incurring ‘catastrophic’ costs due to TB by 2025. This paper examines, by MDR status, the level and composition of costs incurred by TB-affected households during care seeking and treatment; assesses the affordability of TB care using catastrophic and impoverishment measures; and describes coping strategies used by TB-affected households to pay for TB care. (Debora Pedrazzoli, Tropical Medicine and international health 2018)
- Measuring catastrophic costs due to tuberculosis in Viet Nam: Progress towards ending tuberculosis (TB) in Viet Nam includes monitoring the costs borne by patients through periodic facility-based surveys.The proportion of households experiencing catastrophic total costs due to TB in Viet Nam is high, which poses a barrier to TB diagnosis and treatment. Based on study results, programme and partners need to identify key areas for policy action and work towards a national policy guide on intervention to reduce TB patient costs. (N.V. Nhung, The International Journal of Tuberculosis and Lung Disease 2018)
- Measuring the economic burden for TB patients in the End TB Strategy and Universal Health Coverage frameworks: The End TB Strategy promotes both patient-centred TB services and social protection measures, which aim to mitigate the economic hardship faced by TB patients and their households due to direct medical and non-medical expenditures, as well as to lost income. The strategy includes a target that no families should face catastrophic total costs due to TB. The indicator linked to this target aims to capture the total economic burden linked to TB care, and thus differs from the ‘catastrophic expenditure on health’ indicator, a key component of the UHC monitoring framework aligned with the Sustainable Development Goals. Countries, and particularly high TB burden countries, are expected to conduct nationally representative TB patient cost surveys to establish baseline measurements for the catastrophic costs indicator. Findings from these surveys should also help identify entry points for developing policies to ensure better financial and social protection for TB patients. In this paper, we define the key measurable concepts for TB patient cost surveys, notably the types of costs that are captured, and related affordability measures. We discuss methods for measuring these notions in the UHC framework and contrast them with how they are measured in TB patient cost surveys. (Debora Pedrazzoli, The International Journal of Tuberculosis and Lung Disease 2019)
- The Financial Burden of Tuberculosis for Patients in the Western-Pacific Region: The End Tuberculosis (TB) Strategy has the ambitious goal of ending the global TB epidemic by the year 2030, which is aligned to the Sustainable Development Goals. One of three high level indicators of the Strategy is the “catastrophic costs” indicator, which aims to determine the proportion of TB-affected households that incur TB-care related costs equivalent to 20% or more of their annual household income. The target is that zero percentage of TB-affected households will incur catastrophic costs related to TB care by the year 2020. In the Western Pacific Region of the World Health Organization, it is a priority to determine the financial burden of TB and then act to mitigate it. To date, eight countries in the Region have conducted nationally representative TB patient cost surveys to determine the costs of TB care. The results from four countries that have completed these surveys (i.e., Fiji, Mongolia, the Philippines, and Vietnam) indicate that between 35% and 70% of TB patients face catastrophic costs related to their TB care. With these results in mind, significant additional efforts are needed to ensure financial risk protection for TB patients, expand Universal Health Coverage, and improve access to social protection interventions. A multi-sectoral approach is necessary to achieve this ambitious goal by the year 2020. (Kerri Viney, Tropical Medicine and Infectious Disease 2019)
Other Publications:
- Cash interventions to improve clinical outcomes for pulmonary tuberculosis: systematic review and meta-analysis
This study aimed to assess cash transfer interventions for improving treatment outcomes of active pulmonary tuberculosis in low- and middle-income countries. - Effects of social protection on tuberculosis treatment outcomes in low or middle-income and in high-burden countries: systematic review and meta-analysis
The aim of this systematic review was to identify and assess evidences of social protection effects on TB treatment outcomes in low- and middle-income countries or in high TB-burden countries. - Evaluation of a social protection policy on tuberculosis treatment outcomes: A prospective cohort study
This study evaluated the effect of a conditional cash transfer (CCT) policy on treatment success and default rates in a prospective cohort of socioeconomically disadvantaged patients. - Interventions to improve retention-in-care and treatment adherence among patients with drug-resistant tuberculosis: a systematic review
The systematic review aimed to explore interventions to reduce global loss to follow-up (LTFU) during drug-resistant tuberculosis (DR-TB) treatment. - Active Case Finding Among Marginalised and Vulnerable Populations Reduces Catastrophic Costs Due to Tuberculosis Diagnosis
This study aimed to determine the effect of ACF among marginalised and vulnerable populations on prevalence and inequity of catastrophic costs due to TB diagnosis among TB-affected households when compared with passive case finding. - Active Versus Passive Case Finding for Tuberculosis in Marginalised and Vulnerable Populations in India: Comparison of Treatment Outcomes
This study aimed to determine the relative differences in unfavourable treatment outcomes (death, loss-to-follow-up, failure, not evaluated) of ACF and PCF-diagnosed people. - A comprehensive assessment of universal health coverage in 111 countries: a retrospective observational study
This study measured service coverage by a weighted geometric average of four prevention indicators (antenatal care, full immunisation, and screening for breast and cervical cancers) and four treatment indicators (skilled birth attendance, inpatient admission, and treatment for acute respiratory infection and diarrhoea), financial protection by the incidence of catastrophic health expenditures (those exceeding 10% of household consumption or income), and a country’s UHC performance as a geometric average of the service coverage index and the complement of the incidence of catastrophic expenditures.
Jay Achar
Medecins sans Frontieres
Sweden
jay.achar@london.msf.org
Peter Allebeck
Swedish Research Council for Health, Working life and Welfare & Department of Public Health Sciences, Karolinska Institutet, Stockholm, Sweden
Peter.Allebeck@ki.se
Kristi Sidney Annerstedt
Karolinska Institutet
Sweden
Salla Atkins
Tampere University
Finland
Salla.Atkins@tuni.fi
Ines Garcia Baena
World Health Organization
Switzerland
garciabaenai@who.int
Prerna Banati
UNICEF Office of Research – Innocenti
Florence, Italy
pbanati@unicef.org
Dorsjsuen Bayarsaikhan
World Health Organization
Geneva, Switzerland
BayarsaikhanD@who.int
Anurag Bhargava
Department of Medicine
Yenepoya Medical College
Deralakatte, Mangalore
anuragb17@gmail.com
Olivia Biermann
Karolinska Institutet
Sweden
olivia.biermann@ki.se
Delia Boccia
London School of Hygiene and Tropical Medicine
London, United Kingdom
Delia.Boccia@lshtm.ac.uk
Bo Burström
Department of Public Health Sciences, Karolinska Institutet
Stockholm, Sweden
Bo.burstrom@ki.se
Xu Caihong
National Center for TB Prevention and Control
China
xuch@chinacdc.cn
Daniel Carter
London School of Hygiene and Tropical Medicine
London, United Kingdom
Daniel. Carter@lshtm.ac.uk
Maxine Caws
Liverpool School of Tropical Medicine
United Kingdom
mcaws@hotmail.com
Francis Farai Chikuse
Pathcare, Clinical Pathology
francis.chikuse@gmail.com
Hongjo Choi
Korean Institute of Tuberculosis
South Korea
h.choi.kit@gmail.com
Sejin Choi
Ministry of Justice, Republic of Korea
sj.peter.choi@gmail.com
Ana Ciobanu
National TB Control Programme Republic of Moldova
Anna.ciobanu@gmail.com
Amy Collins
Global TB programme
World Health Organization
Geneva, Switzerland
collinsa@who.int
Johan Dahlstrand
Swedish Institute for Global Health Transformation (SIGHT)
Sweden
johan.dahlstrand@kva.se
Vinod Diwan
Department of Public Health Sciences
Karolinska Institutet
Stockholm, Sweden
vinod.diwan@ki.se
Jennifer Dowd
Kings College University
London, United Kingdom
jennbeamdowd@gmail.com
Carlton Evans
Innovation For Health And Development, Imperial College London
Universidad Peruana Cayetano Heredia
United Kingdom
carlton.evans@ifhad.org
Denise Evans
South Africa
devans@heroza.org
Helen Fletcher
London School of Hygiene and Tropical Medicine
London, United Kingdom
Fletcher@lshtm.ac.uk
Rachel Forse
Friends for International TB Relief (FIT)
Vietnam
rachel.forse@tbhelp.org
Peter Friberg
Swedish Institute for Global Health Transformation (SIGHT)
Sweden
peter.friberg@mednet.gu.se
Johan Fritzell
Aging Research Center (ARC)
Karolinska Institutet
Stockholm, Sweden
johan.fritzell@ki.se
Ahmad Fuady
Faculty of Medicine, Universitas Indonesia
Indonesia
ahmad.fuady01@ui.ac.id
Elvis Gama
Liverpool School of Tropical Medicine
Liverpool,United Kingdom
Elvis.Gama@lstmed.ac.uk
Nguyen Binh Hoa
National TB Programme
Vietnam
Susan van den Hof
KNCV
Netherlands
Zhang Hui
National Center for TB Prevention and Control
China
zhanghui@chinatb.org
Bart Jacobs
GIZ
Cambodia
bart.jacobs@giz.de
Lisa Kawatsu
Research Institute of Tuberculosis
Japan
kawatsu@jata.or.jp
Beatrice Kirubi
Karolinska Institutet, LIME
Sweden
beatrice.kirubi@stud.ki.se
Ulrika Lång
Swedish International Development Cooperation Agency (SIDA)
Sweden
Ulrika.Lang@sida.se
Lieve van Leeuw
South African Medical Research Council
South Africa
Lieve.vanleeuw@mrc.ac.za
Christian Lienhardt
Global TB programme
World Health Organization
Geneva, Switzerland
lienhardtc@who.int
Susanne Lokrantz
Swedish International Development Cooperation Agency (SIDA)
Sweden
Susanne.Lokrantz@sida.se
Knut Lönnroth
Department of Public Health Sciences
Karolinska Institutet, Stockholm, Sweden
Knut.lonnroth@ki.se
Ethel Maciel
Federal University of Espirito Santo Vitoria, Brazil
ethel.maciel@gmail.com
Helga Katharina Mahler
GIZ
Germany
helga.mahler@giz.de
Eunice Mailu
Social Protection and M&E National Tuberculosis, Leprosy and Lung Disease Program
Kenya
mailu.eunice@gmail.com
Enos Masini
National Tuberculosis, Leprosy and Lung Disease Programme
Nairobi, Kenya
emasini32@gmail.com
Rose Wanjiku Ng’ethe
National Tuberculosis, Leprosy and Lung Disease Programme
Nairobi, Kenya
wangethe@gmail.com
Luan Nguyen
Friends for International TB Relief (FIT)
Vietnam
luan.vo@tbhelp.org
Pedroso Nhassengo
Ministry of Health
Mozambique
pedrosoepedro@gmail.com
Nobuyuki Nishikiori
World Health Organization
Switzerland
nishikiorin@who.int
Tia Maria Palermo
State University of New York at Buffalo
Buffalo, NY, USA
tiapaler@buffalo.edu
Sanjay M. Pattanshetty
Manipal University
India
sanjay.pattanshetty@manipal.edu
Debora Pedrazzoli
Liverpool School of Tropical Medicine
United Kingdom
Debora.Pedrazzoli@lshtm.ac.uk
Mikko Perkiö
University of Tampere
Finland
mikko.perkio@uta.fi
Leah Prencipe
UNICEF Office of Research – Innocenti
lprencipe@unicef.org
Andy Ramsay
Scotland
andy.ramsay@st-andrews.ac.uk
Rashmi Rodrigues
St. John’s Medical College
India
rashmijr@gmail.com
Will Rudgard
London School of Hygiene and Tropical Medicine
United Kingdom
willrudgard@hotmail.co.uk
Mauro Sanchez
Federal University of Brasilia
Brazil
mauro.sanchez4@gmail.com
Luciana Servo
Institute for Applied Economic Research (Ipea)
Brazil
luciana.servo@gmail.com
Priya Shete
University of California San Francisco
USA
Priya.Shete@ucsf.edu[/v
Hemant Deepak Shewade
Department of Operational Research, The Union South East Asia
India
hemantjipmer@gmail.com
Noemia Siqueira-Filha
Liverpool School of Tropical Medicine
United Kingdom
Noemia.teixeiradesiqueirafilha@lstmed.ac.uk
Andrew Siroka
World Health Organization
Geneva, Switzerland
sirokaa@who.int
Fabio Veras Soares
UNDP
Brazil
fabio.veras@ipc-undp.org
Bertie Squire
Liverpool School of Tropical Medicine
United Kingdom
Bertie.Squire@lstmed.ac.uk
Sedona Sweeny
London School of Hygiene & Tropical Medicine
sedona.sweeney@lshtm.ac.uk
Annika Sweetland
Columbia University
USA
annika.sweetland@gmail.com
Ewan Tomeny
Liverpool School of Tropical Medicine
United Kingdom
Ewan.Tomeny@lstmed.ac.uk
Göran Tomson
Karolinska Institutet
Sweden
Goran.Tomson@ki.se
Phuong Tran
Karolinska Institutet
Sweden
phuong.tran@ki.se
Kingsley Ukwaja
Federal Teaching Hospital, Abakaliki
Nigeria
ukwajakingsley@yahoo.co.uk
Kerri Viney
Karolinska Institutet
Sweden
kerri.viney@ki.se
Diana Weil
World Health Organization
Switzerland
weild@who.int
William Wells
USAID
USA
wwells@usaid.gov
Marieke van der Werf
European Center of Disease Control and Prevention
Sweden
Marieke.vanderWerf@ecdc.europa.eu
Tom Wingfield
Liverpool School of Tropical Medicine
United Kingdom
tom.wingfield@lstmed.ac.uk
Biao Xu
Karolinska Institutet
China
biao.xu.1@ki.se
Li Xue
National Center for TB Prevention and Control
China
lixue@chinacdc.cn
Talemwa Nalugwa Kabuleta
Uganda Tuberculosis Implementation Research Consortium
Uganda
talemwan@yahoo.co.uk
