The history of antibodies
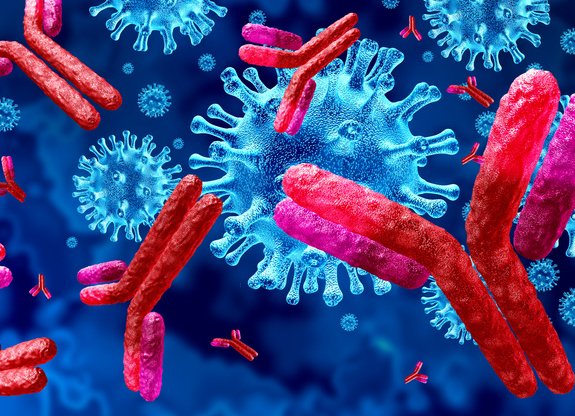
They save lives, but were a long-debated mystery. Antibodies are always ready to protect us against invaders such as bacteria or coronavirus.
Text: Matilda Skoglöw. First published in Swedish in the magazine Medicinsk Vetenskap nr 3/2021.
Facts
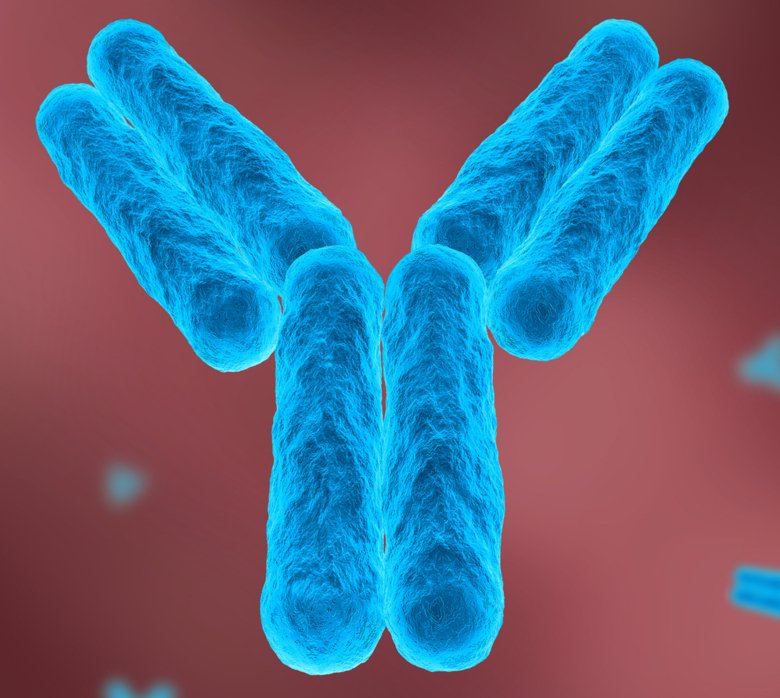
Antibodies are y-shaped proteins that are formed of a special type of white blood cell, known as B cells. The body’s immune system uses antibodies to fight bacteria and viruses, for example. Antibodies bind to foreign substances so that the antibodies or other parts of the immune system can fight the invader.
1890. Serum. Bacteriologists Emil von Behring and Shibasaburo Kitasato in Berlin show that blood from an animal vaccinated against diphtheria can help other animals suffering from the disease to recover. They call the liquid extracted from the blood ‘antitoxin’ and their method ‘serum therapy’.
1894. Horses. In order to start treating diphtheria in humans, larger amounts of antitoxin are needed. Pharmaceutical companies start to immunise sheep and horses to guarantee production. When the treatments are introduced, mortality rates drop dramatically.
1897. Hypothesis. German researcher Paul Ehrlich launches his theory that cells have side chains which can bind to toxins. He is the first to coin the term ‘antibody’ and describe the molecule as ‘branched’.
1905. Side effects. Children treated with large quantities of antitoxin from horses develop a fever, itching and joint pain. The condition is described by Clemens von Pirquet and Béla Schick and is called ‘serum sickness’. The symptoms are caused by the body reacting against the antibodies which are perceived to be foreign.
1923. Mysticism. In the USA, Michael Heidelberger and Oswald Avery discover that antibodies are proteins. Before the discovery, antibodies were seen by most as a mystical substance and their very existence had been debated.
1948. Manufacturing. In his doctoral thesis, Swedish immunologist Astrid Fagraeus describes how the body’s plasma cells are crucial for manufacturing antibodies. Until then, the function of plasma cells had been unknown.
1959. Molecules. Independent of each other, two researchers publish the molecular structure of antibodies. Brit Rodney Porter and American Gerald Edelman are later awarded the Nobel Prize in Physiology or Medicine for their discovery.
1971. ELISA. Swedish researchers Eva Engvall and Peter Perlmann invent the ELISA test which, by identifying and measuring antibodies, reveals the presence of hormones or viruses in the body, for example.
1987. Nobel Prize. How a limited number of genes can produce billions of different antibodies was a mystery solved by Japanese researcher Susumu Tonegawa, who is then awarded the Nobel Prize in Physiology or Medicine. The answer is the random rearrangement of genes, producing new combinations.
2020. Covid. When the coronavirus pandemic strikes the world, antibodies come under the spotlight. In record time, a vaccine for the virus is manufactured and antibody tests are used as a tool to obtain a picture of how the disease spreads in society.
Sources: Llewelyn M.B, Hawkins R.E & S.J. Russell, 1992, ”Monoclonal Antibodies in Medicine: Discovery of Antibodies”, BMJ. Bordon, Y., 2016, ”The many sides of Paul Ehrlich”, Nature Immunology. Nobelprizemuseum.se, ”Kroppens eget försvar” [The Body’s Own Defence]. Historyofvaccines.com, ”Timeline”, The College of Physicians of Philadelphia. Van Epps, Heather L., 2005, ”How Heidelberger and Avery sweetened immunology”, Journal of Experimental Medicine. 1177.se, ”Så fungerar immunförsvaret”[How the Immune System Works]. Absoluteantibody.com, ”A Brief History of Antibodies”. Britannica, ”Tonegawa Susumu”. IAVI.org, ”Broadly Neutralizing Antibodies for HIV Prevention”.
Challenges of the future
Developing monoclonal treatments. Since the discovery of monoclonal antibodies in the 1970s, their use in healthcare has become much more common. Today, monoclonal antibodies are used for treating cancer and autoimmune diseases, for example. Challenges include understanding antibodies even better, developing the technology and successfully treating more diseases.
Vaccine against HIV. The HIV virus mutates exceptionally rapidly, which makes developing a vaccine a challenge. As antibodies are created to attack an invader with specific features, a vaccine quickly loses its effect when the virus changes shape. Research is ongoing on broadly neutralising antibodies which are capable of eliminating many different types of HIV virus and should therefore be able to form the basis of a future vaccine against the disease.

Looking to understand the creator of antibodies
Pia Dosenovic, research assistant at the Department of Microbiology, Tumour and Cell Biology at Karolinska Institute, is working to better understand how B cells function in vaccination.
“B cells are important for protecting us against infection. When you are vaccinated, they start to expand and can then develop different types of functions, like producing antibodies or becoming memory B cells,” she says.
Why B cells develop in a certain direction is still largely unknown, which is something Pia Dosenovic wants to change with her research. With a better basic understanding of B cells, an effective vaccine for HIV, for example, could become a reality. As the HIV virus often mutates, it is currently difficult to develop a durable vaccine.
“We want to activate B cells which respond to parts of the virus which don’t change. But in a normal immune system, these B cells are few and far between; it’s like looking for a needle in a haystack.”
In order to solve the problem, Pia Dosenovic is using genetically-engineered mice. She is also researching alternative ways to design vaccines, using antibodies instead of proteins.
