What is schizophrenia?
Schizophrenia is a severe brain disease of neurodevelopmental origin and is characterized by chronic or relapsing episodes of psychosis.

Approximately half a percent of the worldwide population is estimated to suffer from schizophrenia and the majority experience their first symptoms already in their late teens or in early adulthood. This makes schizophrenia one of the major public health challenges, and the estimated costs for the disease is estimated to be greater than those for all cancers combined.
The clinical presentation shows considerable variability, but the core symptoms typically make a profound impact on thoughts, emotions, and behavior. The diagnosis is criteria based and the diagnostic assessment rely on repeated clinical interviews and mental status examinations. Despite the lack of objective biomarkers, a diagnosis of schizophrenia shows considerable stability over time.
Continuous antipsychotic medication is the mainstay of treatment for schizophrenia. However, disabling symptoms persist in many patients, and some suffer from unwanted side effects.
Genetic risk factors are the main cause of schizophrenia and unbiased large-scale genetic studies have identified a growing number of variations in the DNA sequence that associates with schizophrenia. Several environmental risk factors have also been identified. These include maternal immune activation as well as use of cannabis.
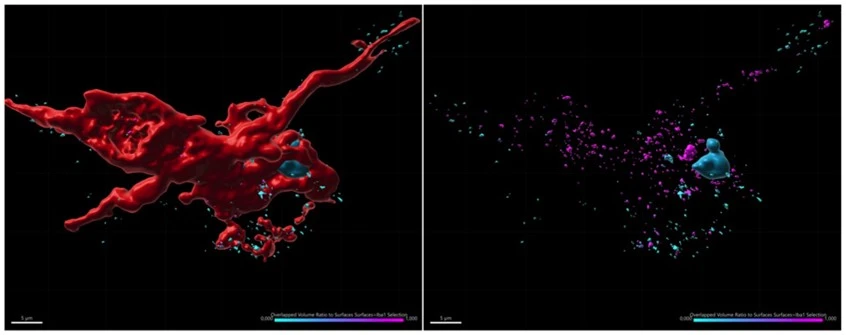
Large brain imaging studies and repeated investigations of brain tissue obtained from deceased individuals with schizophrenia have revealed indisputable structural brain abnormalities. Foremost, a reduction in frontal cortical thickness have been observed and can largely be explained by a loss of connections between the nerve cells, the so-called synapses.
Investigations to understand how risk factors causes brain changes and symptoms in the patients are ongoing but much of the pathophysiology remains elusive. However, with such knowledge more precise and personalized drug targeting is possible.
KaSP - Schizophrenia history
Schizophrenia is believed to have accompanied mankind through history. However, it took until 1887 before the disease was given its own identity by Dr. Emile Kraepelin in 1887.
The disease is mentioned in documents that can be traced to the ancient Pharaonic Egypt. At that time it was supposed that mental disorders, in general, were caused by an evil possession of the body, and as a consequence, the appropriate treatment was exorcising of demons.
The German physician, Emile Kraepelin was the first to classify mental disorders into various categories. He used the term "dementia praecox" for individuals with symptoms that we now associate with schizophrenia.
Eugen Bleuler, a Swiss psychiatrist, changed the name of the disease to "schizophrenia" in 1911 since it was obvious that Kraepelin's name “dementia praecox” was misleading. The name schizophrenia originates from the Greek roots “schizo” (split) and “phrene” (mind) and was ment to reflect the disoriented thinking of individuals with the disorder. Bleuler was also the first to describe the symptoms of the disease terms of "positive" or "negative." The disease is nowadays defined according to the criteria of DSM-5.
For many years effective pharmacological treatment was lacking. The first medicines were developed during the 1950s, one of the first was haloperidol (1958). This drug was one of several substances known as the first-generation antipsychotics, and many of these drugs are still in use. During the 1970s new drugs with more beneficial side effects were introduced, for example, clozapine, known as one the most efficient antipsychotics.
