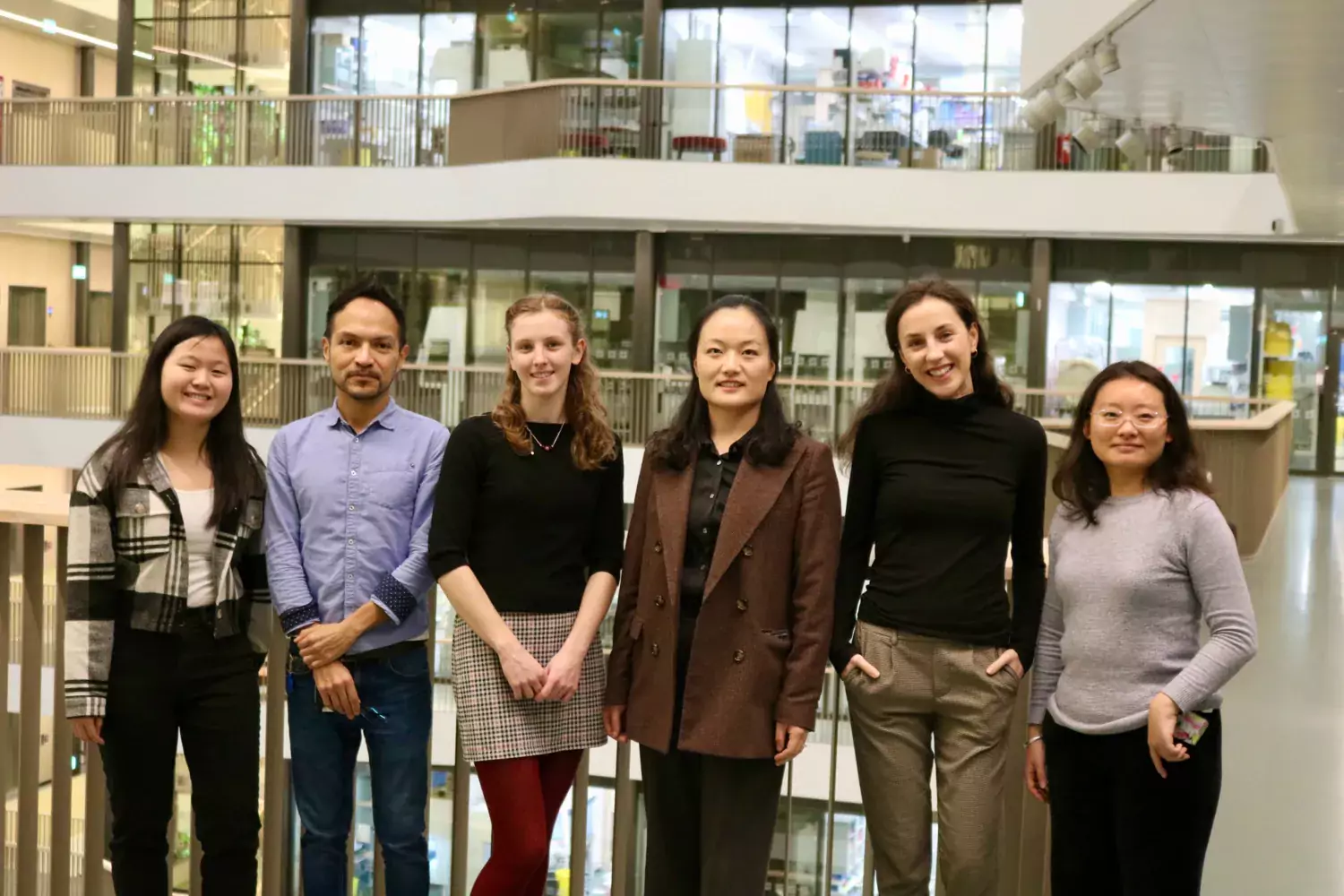
Lars Engstrand group
In the Engstrand group, we have established a highly effective translational scientific environment, with a broad interdisciplinary approach to the interface between epidemiology and the microbiological, immunological and genetic aspects of chronic diseases. Our goal is to clarify the pathogenic mechanisms within the fields of gastroenterology, women’s health and cancer, define what is a normal and healthy microbiome, and to improve the prospects for primary prevention.
Lars Engstrand is heading the division, and Microbiome Exploration, Development for Intervention, MEDI, consists of:
Culturomics - Valerie Valeriano
Bioinformatics – Fredrik Boulund
Labcore – Maike Seifert
Project Management and Support – Marica Ekström
Womans Health – Ina Schuppe Koistinen.
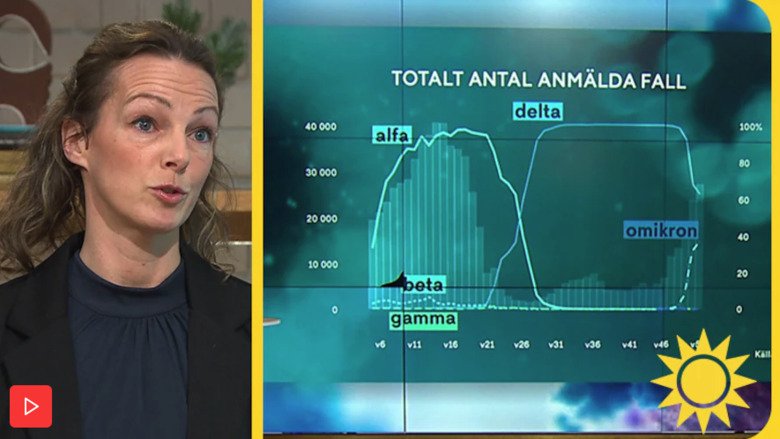
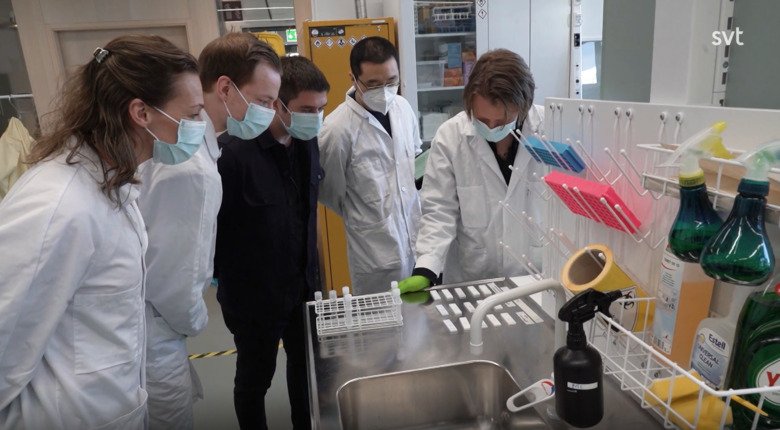
The division also includes National Pandemic center NPC – Jessica Alm, as well as the labs of Amir Saei and Juan Du.