Timeline: A bumpy ride toward good treatments for Parkinson's disease
Tremors, slowed movement, stiffness and symptoms that are not visible. For thousands of years, Parkinson’s disease has been affecting people’s lives, and yet there is still no cure.
Text: Matilda Skoglöw for the magazine Medicinsk Vetenskap No 1/2022, in translation from Swedish
Parkinson’s disease is our second most common neurological disease, after Alzheimer’s disease, with roughly 6 million people diagnosed worldwide. The diagnosis is based on symptoms such as reduced mobility, stiffness and tremors. The motor symptoms found in this disease are caused by a slow destruction of nerve cells in the brain that produce dopamine. Follow the timeline for Parkinson's disease:
1000 years B.C Ayurveda. Symptoms indicative of Parkinson’s disease are described in Charaka Samhita, a text on the Indian medicine of healing called Ayurveda. Similar descriptions can be found in other antique documents from, for example, China and the Roman empire.
1817 Debut book. British physician James Parkinson publishes the book An Essay on the Shaking Palsy. It is the first detailed description of the disease that will later be named after him.
1872 Naming. French neurologist Jean-Martin Charcot suggests the name Parkinson’s disease and describes slowed movement as one of the main symptoms.
1886 Risk group. Physician William Richard Gowers highlights the fact that men are at a greater risk of being diagnosed with Parkinson’s disease. He describes his patients and, among other things, recommends hemlock and cannabis as ways to treat tremors.
1912 Accumulation. In Germany, physician Fritz Heinrich Lewy discovers abnormal clusters of proteins in the brain in people who have died as a result of Parkinson’s. These clusters are later named Lewy bodies and are also found to be linked to dementia.
1919 The midbrain. Substantia nigra is the first section of the brain that has been linked to Parkinson’s disease. The majority of the brain’s dopamine-producing nerve cells can be found in this area. Researcher Konstantin Tretiakoff is one of the people behind this discovery.
1916 Dopamine deficiency and medicine. Ehringer and Hornykiewicz demonstrate that people who have died from Parkinson’s had a serious lack of dopamine in their brains. The following year, L-Dopa is administered to patients for the first time, a medicine that is converted into dopamine once it is in the body.
1997 Deep brain stimulation. It is demonstrated that high frequency brain stimulation of specific brain structures can result in substantial symtom relief in cases of severe Parkinson’s.
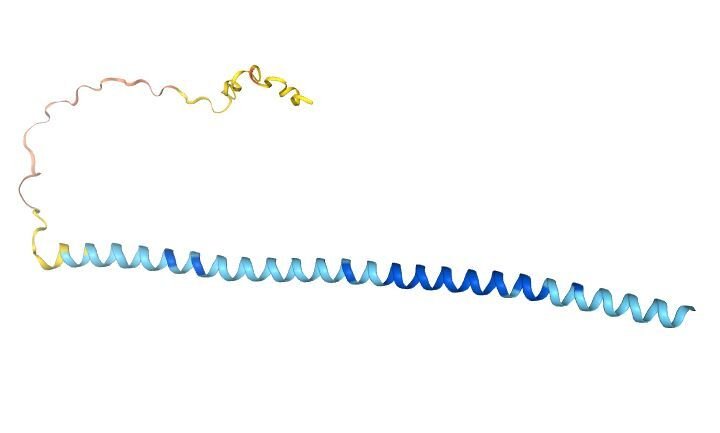
1997 Heredity and alpha-synuclein. The protein alpha-synuclein becomes the first genetic factor to be identified as a cause of Parkinson’s. This discovery is made through studies of an Italian family and Greek family where the disease is hereditary. That same year, it is discovered that alpha-synuclein is a main component in Lewy bodies.
2000 Nobel prize. Swedish pharmacologist Arvid Carlsson was awarded the Nobel Prize of Physiology or Medicine for his discovery from 1958: that dopamine is a signal substance in the brain. This discovery contributed to L-Dopa treatment against Parkinson’s.
2020s Stem cells. A research group reports that it is carrying out an initial attempt to transplant stem cells to the brain of a man who suffers from Parkinson’s. The stem cells were harvested from the man himself and turned into dopamine-producing cells.
Future challanges
Better understanding of non-motor symptoms
One future challenge is to develop an understanding and treatment of non-motor symptoms such as impaired sleep, depression or vulnerability to stress.
Development of disease-modifying therapies
With a medicine that slows down the disease progression itself, treatment could be introduced at an early stage. It could also open up to screening of patients with a genetically enhanced risk of developing Parkinson’s disease. A future challenge will also be to restore the nerve cells that have been lost since the patient became sick. This has been successfully achieved in animal models of Parkison’s disease.
The development of physical exercise programs
Studies at, for example, Karolinska Institutet have shown that physical activity may work as a supplement to medicine and reduce problems with balance and walking, to name just a few. However, increased knowledge is needed in terms of what type and amount of physical exercise produces the greatest effects.
Sources
‘The History of Parkinson’s Disease: Early Clinical Descriptions and Neurological Therapies’, 2011, Cold Spring Harbor Perspectives in Medicine, Goetz CG, ‘Milestones of Parkinson’s Disease Research: 200 Years of History and Beyond’, 2017, Neuroscience Bullentin, Li S & Le W, ‘ A secret experiment revealed: In a medical first, doctors treat Parkinson’s with a novel brain cell transplant’, 2020, Begley S, STAT, ‘Parkinsons sjukdom – heterogen och komplex i sitt kliniska uttryck’, 2020, Läkartidningen, thescienceofparkinsons.com.
